How to Personalize Melatonin Use for Better Sleep (Sleep Problems ≠ Melatonin Problems)
We have looked at why so many adults wake after 5-6 hours even when sleep hygiene is solid. Melatonin often enters that conversation as an easy next step—but it infrequently solves the problem outright.
Its effects depend on timing, metabolism, and whether melatonin is even the limiting factor for you.
If you’re using melatonin — or considering it — this article unpacks the most common pitfalls to avoid.
Just as important, it will help you assess whether melatonin is the right fit for supporting your sleep in the first place.
And, if it is, how to personalize your approach so you can capture the benefits without the unintended metabolic side effects.
Here’s what we’ll walk through together:
- The 3 overlooked reasons melatonin use is more complex than just shifting it earlier or later
- How to individualize your melatonin approach so it supports sleep while minimizing metabolic disruption
- The Underused Tool: Four-Point Melatonin Profiling
- When to redirect focus to other drivers of disrupted sleep.
Let’s get started.
3 Reasons Melatonin Use Is More Complex Than Just Taking It Earlier or Later — or Avoiding Late Meals
1. Sleep Problems ≠ Melatonin Problems
Melatonin is rarely the primary (or only) driver of the sleep issues many individuals experience.
3 a.m. awakenings, fragmented sleep patterns, or mornings where sleep unrefreshing despite adequate sleep time often stem from other factors—or a combination of them.
To name a few:
- Autonomic regulation: poor balance between “fight-or-flight” and “rest-and-recover” can prevent full transition into restorative sleep.
- Hormones: testosterone decline, perimenopause, and menopause alter sleep architecture independent of melatonin function.
- Sleep apnea, restless legs, or medication can create additional disruption.
In these cases, adding melatonin may temporarily mask symptoms without addressing the underlying cause.
2. Age Doesn’t Predict Individual Melatonin Needs
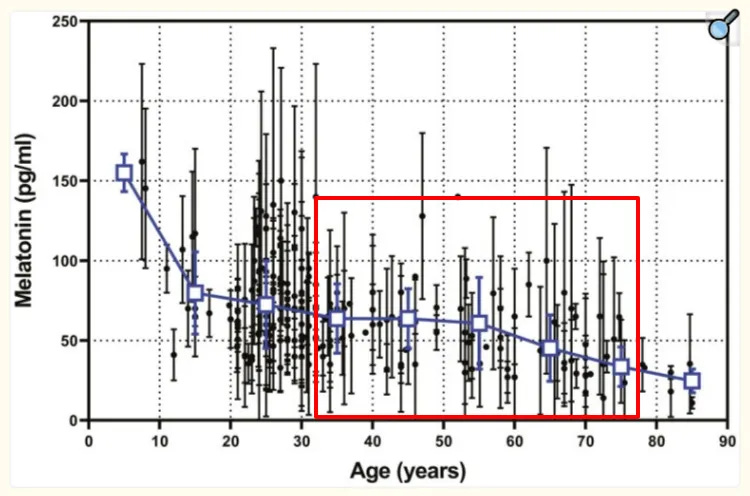
While average melatonin production declines with age, individual variation is large.
In my experience reviewing melatonin profiles, some individuals in their 70s still maintain strong night patterns, while others in their 40s already show weaker or irregular patterns.
Chronotype, genetics, health status, and light exposure history influence melatonin biology as much as age alone.
Supplementing purely “because of age” risks creating a problem where none existed, exposing individuals to unnecessary hormone load while overlooking the true cause of poor sleep.
3. Individual Melatonin Timing Varies by Up to 4–5 Hours Between People
Even when melatonin supplementation is appropriate, the “when” isn’t universal.
Your biological night is determined by your internal circadian system, not wall-clock time.
When melatonin support helps differs between individuals—sometimes by as much as 4–5 hours, even for the same target bedtime.
For example:
- Individuals with a morning-type chronotype often show earlier biological night signals than those with evening-type chronotypes, even when they keep the same bedtime.
- Medications such as beta-blockers have been shown to suppress melatonin secretion, while some antidepressants can alter its clearance. These effects change the timing window in which supplemental melatonin would interact with the body’s own rhythm.
So the challenge isn’t whether melatonin works—it’s how well the approach is tailored to the person using it.
That shift from universal rules to personal alignment is where we turn next.
If you’d like to go deeper, my 21-day melatonin sleep recovery blueprint
If you are already using melatonin but still getting unpredictable results—some nights it helps, others it does not—it is easy to end up increasing the dose, switching brands, and spending more without a better outcome. Over time, that pattern delivers the worst combination: inconsistent sleep, ongoing expense, and higher risk of morning grogginess and impaired glucose handling.
The 21-Day Melatonin Sleep Recovery Blueprint + Decision Matrix is designed to end that uncertainty—without requiring lab testing. In 21 days, you follow a structured sequence to:
- determine whether melatonin is actually relevant to your sleep pattern or was never the right lever in the first place
- adjust timing and dose in a physiologically aligned way, so you are not relying on guesswork or chronic high doses
At the end of the 21 days, the 21-Day Melatonin Sleep Recovery Blueprint + Decision Matrix, gives you enough data to make a clear decision: continue with an optimized melatonin plan, or stop investing in a supplement that is not meaningfully improving your sleep.
You can get it here:
How to Personalize Your Melatonin Approach
The same 9 p.m. melatonin dose might align with one person’s biological night while falling outside the optimal biological window for another.
- From a circadian perspective, melatonin only supports sleep when it matches your internal night. When mistimed, it can reinforce the wrong phase of night, producing fragmented sleep or 3 a.m. awakenings instead of continuity. Mechanistically, supplemental melatonin interacts with the circadian pacemaker, and if shifted, it destabilizes rather than stabilizes sleep.
- From a metabolic perspective, it should not overlap with active food processing.
Both constraints are individual —which means universal timing advice is insufficient.
Even with these considerations in mind, the most fundamental question remains:
Are your sleep problems caused by melatonin?
The next step is not to try a new dose or formulation.
It’s to determine whether melatonin is relevant to your sleep at all, and only then to align timing and amount with your biology.
Many of us end up experimenting—changing brands, adjusting dosage, shifting it earlier or later—only to find the results are marked by 3 a.m. awakenings or temporary.
There is a more precise approach.
The Underused Tool: Four-Point Melatonin Profiling
Until recently, the ability to map melatonin rhythms was available mainly to research labs and specialized circadian medicine centers. For years, it remained impractical for most individuals outside those settings.
That landscape has shifted.
What was once locked in research settings is now available to consumers through multi-sample saliva profiles. Instead of a one-off blood test, these profiles capture hormone levels across the day and early night—revealing when your system initiates and maintains its nocturnal signal — the physiological window where melatonin naturally coordinates sleep timing.
Few people know this exists, and fewer realize how it can transform decision-making: clarifying whether supplementation is relevant, identifying personal timing, and guiding dosing so melatonin enhances sleep instead of disrupting it.
Standard sleep evaluations—even those costing thousands—often measure everything except the timing of the hormone that sets the circadian night.
💡 Even the most advanced sleep clinics focus heavily on breathing and movement data. Yet without melatonin profiling, they miss the hormone cue that defines circadian night — identifying both its timing and whether the circadian signal is adequately generated and maintained.
Here’s how a 4-point melatonin profile test can help you determine whether melatonin is contributing to your sleep issues and how to align it with timing and dosing so it supports, rather than fragments, your rest:
1. Confirms relevance.
A normal profile—showing a healthy rise and sustained levels through the night—suggests melatonin is not your weak link.
In that case, supplementation is unlikely to provide benefit.
This redirection is valuable: it saves you both time and the cumulative expense of supplements that may never have been necessary in pursuit of an ineffective approach that may, in some cases, disrupt sleep.
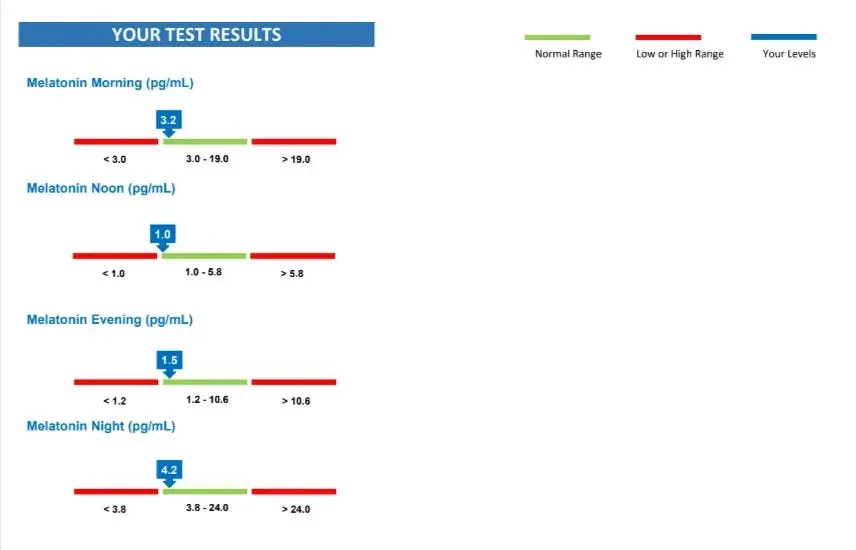
2. Personal timing.
A profile reveals the timing of your own biological night, so support can be matched to that window rather than a universal “take it 5-30 minutes before sleep” rule.
In my experience, when individuals report that melatonin “doesn’t work,” the issue is often a timing mismatch—taking the right substance at the wrong point in their circadian rhythm. This is one of the main reasons why melatonin doesn’t help even when someone might genuinely need it.
3. Dose guidance.
- If your profile shows adequate nighttime levels, layering on high doses only raises the risk of morning grogginess and impaired post-breakfast glucose control.
- If your profile shows a weak rise, then the evidence favors minimal, physiologic replacement—below most over-the-counter products.
Either way, a single profile (this is the one I use) clarifies both relevance and dosing, replacing repeated trial and error with a straightforward path forward.
The Practical Takeaway: A profile provides closure—if melatonin isn’t the issue, you can redirect focus to other drivers of disrupted sleep.
If it is, you know when and how much to use, without exceeding what is physiologically needed.
At the same time, I know not everyone wants to or can test right away.
Some of you might want something practical you can use tonight rather than waiting for a kit, collection, and results.
That’s where structured adjustments come in.
(They aren’t as precise as profiling, but they offer a safer and informed starting point than unguided trial and error.)
- For some, these adjustments will bring melatonin back into alignment with circadian timing and help stabilize sleep.
- For others, they will reveal that melatonin isn’t the weak link, redirecting focus toward autonomic, circadian, or hormone support instead.
Either way, the benefit is the same: you move forward with clarity.
Warmly,
—Kat
P.S. If melatonin is relevant to your sleep disruption:
Many adults find melatonin disappointing. Here are the 5 safe, structured adjustments you can apply tonight to improve sleep—without increasing the dose.
👉 Why Melatonin Often Fails (& 5 Safe Adjustments for Better Sleep) →
If melatonin isn’t your primary sleep issue:
If you’ve read this far and feel your sleep challenges fall outside melatonin’s role, you can continue with the resources that address other patterns of disrupted sleep.
👉 Explore other root-cause systems that affect sleep →
Sleep OS Hormones is now available as a 60-day self-guided program with dedicated systems for estrogen, progesterone, and testosterone, or bundled together for a more complete approach.
References
- Kennaway DJ. The dim light melatonin onset across ages, methodologies, and sex and its relationship with morningness/eveningness. Sleep. 2023 May 10;46(5):zsad033.
- Deacon S and Arendt J (1995) Melatonin-induced temperature suppression and its acute phase-shifting effects correlate in a dose-dependent manner in humans. Brain Res 688 (1–2), 77–85.
- Tordjman S, Chokron S, Delorme R, Charrier A, Bellissant E, Jaafari N, Fougerou C. Melatonin: Pharmacology, Functions and Therapeutic Benefits. Curr Neuropharmacol. 2017 Apr;15(3):434-443.
- Li J, Somers VK, Xu H, Lopez-Jimenez F, Covassin N. Trends in Use of Melatonin Supplements Among US Adults, 1999-2018. JAMA. 2022 Feb 1;327(5):483-485.
- Konstandi M, Johnson EO. Age-related modifications in CYP-dependent drug metabolism: role of stress. Front Endocrinol (Lausanne). 2023 May 24;14:1143835.
- Waldhauser F, Kovács J, Reiter E. Age-related changes in melatonin levels in humans and its potential consequences for sleep disorders. Exp Gerontol. 1998 Nov-Dec;33(7-8):759-72.
- Burgess HJ, Park M, Wyatt JK, Rizvydeen M, Fogg LF. Sleep and circadian variability in people with delayed sleep-wake phase disorder versus healthy controls. Sleep Med. 2017 Jun;34:33-39.
- Gooneratne NS, Edwards AY, Zhou C, Cuellar N, Grandner MA, Barrett JS. Melatonin pharmacokinetics following two different oral surge-sustained release doses in older adults. J Pineal Res. 2012 May;52(4):437-45.
- Tuft C, Matar E, Menczel Schrire Z, Grunstein RR, Yee BJ, Hoyos CM. Current Insights into the Risks of Using Melatonin as a Treatment for Sleep Disorders in Older Adults. Clin Interv Aging. 2023 Jan 12;18:49-59.
- Peneva, V.M.; Terzieva, D.D.; Mitkov, M.D. Role of Melatonin in the Onset of Metabolic Syndrome in Women. Biomedicines 2023, 11, 1580.
- Tuomi T, Nagorny CLF, Singh P, Bennet H, Yu Q, Alenkvist I, Isomaa B, Östman B, Söderström J, Pesonen AK, Martikainen S, Räikkönen K, Forsén T, Hakaste L, Almgren P, Storm P, Asplund O, Shcherbina L, Fex M, Fadista J, Tengholm A, Wierup N, Groop L, Mulder H. Increased Melatonin Signaling Is a Risk Factor for Type 2 Diabetes. Cell Metab. 2016 Jun 14;23(6):1067-1077
- Garaulet M, Qian J, Florez JC, Arendt J, Saxena R, Scheer FAJL. Melatonin Effects on Glucose Metabolism: Time To Unlock the Controversy. Trends Endocrinol Metab. 2020 Mar;31(3):192-204.
- Garaulet M, Gómez-Abellán P, Rubio-Sastre P, Madrid JA, Saxena R, Scheer FA. Common type 2 diabetes risk variant in MTNR1B worsens the deleterious effect of melatonin on glucose tolerance in humans. Metabolism. 2015 Dec;64(12):1650-7.
- Garaulet M, Qian J, Florez JC, Arendt J, Saxena R, Scheer FAJL. Melatonin Effects on Glucose Metabolism: Time To Unlock the Controversy. Trends Endocrinol Metab. 2020 Mar;31(3):192-204.
- José Cipolla-Neto, Fernanda Gaspar do Amaral, Melatonin as a Hormone: New Physiological and Clinical Insights, Endocrine Reviews, Volume 39, Issue 6, December 2018, Pages 990–1028
- Savage RA, Zafar N, Yohannan S, et al. Melatonin. [Updated 2024 Feb 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.
- Rubio-Sastre P, Scheer FA, Gómez-Abellán P, Madrid JA, Garaulet M. Acute melatonin administration in humans impairs glucose tolerance in both the morning and evening. Sleep. 2014 Oct 1;37(10):1715-9.
- Lauritzen ES, Kampmann U, Pedersen MGB, Christensen LL, Jessen N, Møller N, Støy J. Three months of melatonin treatment reduces insulin sensitivity in patients with type 2 diabetes-A randomized placebo-controlled crossover trial. J Pineal Res. 2022 Aug;73(1):e12809.
- C.J. Morris, J.N. Yang, J.I. Garcia, S. Myers, I. Bozzi, W. Wang, O.M. Buxton, S.A. Shea, & F.A.J.L. Scheer, Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans, Proc. Natl. Acad. Sci. U.S.A. 112 (17) E2225-E2234
- Cajochen C, Münch M, Knoblauch V, Blatter K, Wirz-Justice A. Age-related changes in the circadian and homeostatic regulation of human sleep. Chronobiol Int. 2006;23(1-2):461-74
- Skene DJ, Swaab DF. Melatonin rhythmicity: effect of age and Alzheimer’s disease. Exp Gerontol. 2003 Jan-Feb;38(1-2):199-206.
- Reiter, R.J.; Sharma, R.; Chuffa, L.G.d.A.; Simko, F.; Dominguez-Rodriguez, A. Mitochondrial Melatonin: Beneficial Effects in Protecting against Heart Failure. Life 2024, 14, 88.
- Sletten TL, Vincenzi S, Redman JR, Lockley SW, Rajaratnam SM. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010 Nov 1;1:137.
- Baskett JJ, Broad JB, Wood PC, Duncan JR, Pledger MJ, English J, Arendt J. Does melatonin improve sleep in older people? A randomised crossover trial. Age Ageing. 2003 Mar;32(2):164-70. doi: 10.1093/ageing/32.2.164. PMID: 12615559.
- Buscemi N, Vandermeer B, Pandya R, Hooton N, Tjosvold L, Hartling L, Baker G, Vohra S, Klassen T. Melatonin for Treatment of Sleep Disorders. Evidence Report/Technology Assessment No. 108. (Prepared by the University of Alberta Evidence-based Practice Center, under Contract No. 290-02-0023.) AHRQ Publication No. 05-E002-2. Rockville, MD: Agency for Healthcare Research and Quality. November 2004.
- Marupuru S, Arku D, Campbell AM, Slack MK, Lee JK. Use of Melatonin and/on Ramelteon for the Treatment of Insomnia in Older Adults: A Systematic Review and Meta-Analysis. J Clin Med. 2022 Aug 31;11(17):5138.
- Ferracioli-Oda E, Qawasmi A, Bloch MH. Meta-analysis: melatonin for the treatment of primary sleep disorders. PLoS One. 2013 May 17;8(5):e63773.
- Fu, K. (2025, June 6). The 3 forms of sleep disruption that shrink your brain—and how to tell if your sleep is actually protecting you from cortical atrophy, brain shrinkage and neurodegeneration. The Longevity Vault.
- Fu, K. (2025, June 12). Melatonin for sleep: Why it often fails—and what to do instead to stay asleep to prevent brain aging, cognitive decline, and toxin buildup at night. The Longevity Vault.
- Fu, K. (2025, July 29). The 2 metabolic systems melatonin disrupts—even in healthy adults. The Longevity Vault.
- Fu, K. (2025, September 10). Melatonin as a longevity molecule? Safety data, metabolic risks, and antioxidant promise. The Longevity Vault.
- Fu, K. (2025, September 16). Melatonin can impair blood sugar regulation (& what this means for your melatonin use). The Longevity Vault.
- Benloucif S, Burgess HJ, Klerman EB, Lewy AJ, Middleton B, Murphy PJ, Parry BL, Revell VL. Measuring melatonin in humans. J Clin Sleep Med. 2008 Feb 15;4(1):66-9.
- Arendt J, Aulinas A. Physiology of the Pineal Gland and Melatonin. [Updated 2022 Oct 30]. In: Feingold KR, Ahmed SF, Anawalt B, et al., editors. Endotext [Internet]. South Dartmouth (MA):
- Nogueira LM, Sampson JN, Chu LW, Yu K, Andriole G, Church T, Stanczyk FZ, Koshiol J, Hsing AW. Individual variations in serum melatonin levels through time: implications for epidemiologic studies. PLoS One. 2013 Dec 23;8(12):e83208.


