Should You Supplement Vitamin D Regardless of Diet? A Newly Published Case Report (September 2025) Of Acute Kidney Failure Shows Why You Shouldn’t: Vitamin D Supplementation Risks
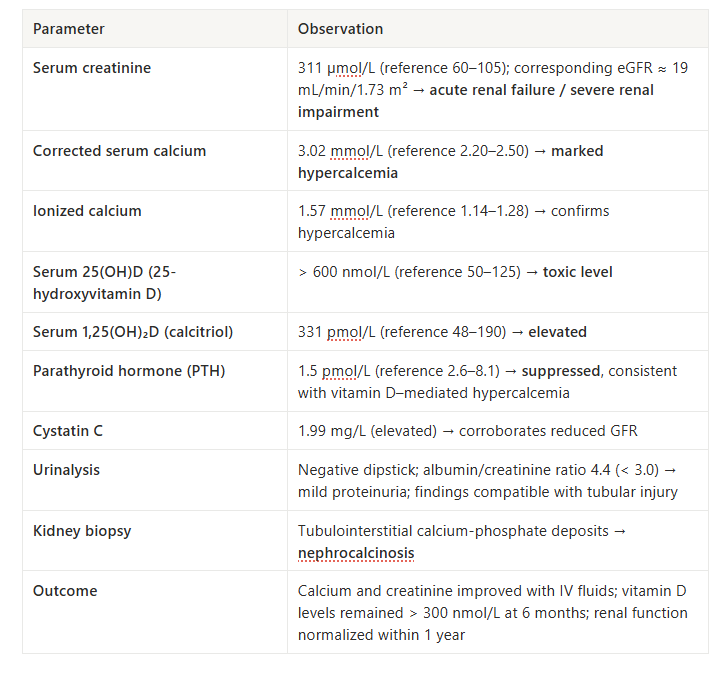
A middle-aged man, previously healthy, presented at the hospital with acute kidney failure after 6 months of vitamin D supplementation.
His daily dose: ~4,800 IU, purchased online and self-prescribed —about six times higher than the Nordic safe limit (since the case originated in Norway) and slightly above the 4,000 IU/day U.S.–EU upper limit.
The result: serum calcium levels reached 3.02 mmol/L (normal range ≈ 2.15–2.55 mmol/L), kidney function declined sharply (eGFR ≈ 19 mL/min, normal ≥ 90 mL/min), and a renal biopsy showed calcium-phosphate deposits in the tubular tissue.
Treatment required intravenous fluids and discontinuation of vitamin D. It took roughly a year before his kidney function recovered.
This case, just published on September 23, 2025 in The Journal of the Norwegian Medical Association, demonstrates an important pattern: what many consider a moderate supplementation dose can lead to medically adverse outcomes when taken without monitoring serum levels.
The patient never tested his vitamin D. He assumed the dose was reasonable.
Over 6 months, the cumulative effect caused kidney damage—because his body metabolized and responded to that dose differently than average models might predict.
A Great Question I Recently Received: “Should we supplement vitamin D regardless of our food logs?”
This question came from a health-conscious individual who already tracks their vitamin D intake through food logs but wonders whether they should supplement anyway—even if their diet appears to provide enough.
The short answer is no—not without testing your serum levels first.
Dietary intake alone tells us very little, if anything, about our circulating vitamin D concentration. The relationship between ingested dose and resulting blood levels differ considerably from one person to another.
Sunlight also contributes, but its effect depends on latitude, season, skin type, and time outdoors, so it does not provide a reliable baseline by itself.
Some individuals can take 1,000 IU daily and reach optimal range. Others take 20,000 IU and remain deficient. And some—like the health man in the September 2025 case study—take under 5,000 IU and develop hypercalcemia.
The issue isn’t the dose itself. It’s how your body converts, transports, and responds to vitamin D.
Vitamin D Supplementation Risks: Why Vitamin D Metabolism Varies So Much
Individual response to vitamin D supplementation is influenced by several processes that differ substantially across populations.
Genetic polymorphisms affect conversion, transport, and cellular response.
Three key genes contribute to this variability:
➤ VDR — the vitamin D receptor gene. It determines how strongly cells respond to calcitriol, the active hormone form of vitamin D.
➤ GC — the gene that encodes vitamin D–binding protein, which governs how vitamin D is transported through the bloodstream and delivered to tissues.
➤ CYP2R1 — a key hydroxylase enzyme that converts vitamin D₃ from sunlight or diet into 25-hydroxy-vitamin D, the circulating form measured to assess vitamin D status.
Research shows that individuals with multiple risk alleles in these genes are up to 2× more likely to remain deficient despite standard supplementation. These variants are common across many populations globally.
Data from large-scale studies show that deficiency rates remain high even in regions with abundant year-round sunshine. In India, Pakistan, and Bangladesh, over 80% of adults are deficient. In Iran and Turkey, 67–90% of older adults fall below recommended levels.
Therefore sun exposure alone—or dietary intake alone—cannot reliably predict serum vitamin D status. Genetic background, skin type, age, gut absorption, and seasonal patterns all contribute to individual differences.
Co-nutrients also matter.
Magnesium is required for each enzymatic activation step, and vitamin K₂ directs calcium into bone rather than arteries or kidneys. Low magnesium can make supplementation appear “ineffective,” while low K₂ can increase calcification risk when intake is high.
What this means in practice:
Another person’s optimal dose may be inadequate—or excessive—for you.
Online calculators that estimate “X IU will produce Y nmol/L” provide rough guidance, but individual responses can vary by 30–70 nmol/L from these predictions.
The only way to know where you fall is to measure it.
How I Optimized My Vitamin D Levels
I used to assume I was approaching this correctly—taking D3 supplements, getting sunlight when possible. Then winter arrived. My test repeatedly came back ~30 nmol/L.
I adjusted my dose upward. The next test showed 150 nmol/L—above my target range.
It took 5 Vitamin D tests in 2023 to figure out what worked for my biology, intake levels, genetics and seasonal changes. The magnitude of seasonal variation was larger than I expected, and standard dosing recommendations didn’t account for my response pattern.Vitamin D overdose
Testing revealed something I couldn’t have predicted through calculation.
Once I understood my response pattern, I was able to design a dosing strategy that keeps me in my target range year-round. But I only reached that point through some rounds of lab work and adjustment.
Because I’ve now characterized my personalized response, I monitor it at ~2x a year—late winter and early autumn—so the fine tunings are personalized and data-driven rather than seasonal trial-and-error.
Upgrade for personalized roadmaps—systematic implementation frameworks you can personalize to your specific biomarkers and risk factors.
Vitamin D Supplementation Risks: The 20,000–30,000 IU Vitamin D Trend
As winter approaches in the Northern Hemisphere, vitamin D supplementation becomes a common topic again.
I’ve heard from many individuals who take 20,000–30,000 IU daily—often without testing their levels.
The reasoning usually runs: “I live in a northern climate with limited winter sun, so I need high doses to compensate” or “I want to be in the upper range for optimal health.”
This case study shows how this approach can lead to adverse outcomes.
The patient took 4,800 IU—far less than 20,000—and developed hypercalcemia severe enough to impair kidney function. His symptoms (fatigue, thirst, nausea) overlapped with dozens of other conditions, making early detection difficult.
Vitamin D does not follow a linear “more is better” relationship.
Research indicates an inverted U-shaped curve:
- Too low → inflammation, poor sleep, cognitive decline
- Too high → disrupted calcium signaling, cognitive impairment over time, kidney stress
The optimal range is narrower than many assume.
High-dose supplementation without testing means you’re operating without feedback.
You may be correcting a deficiency, maintaining an adequate level, or gradually accumulating excess. Without measurement, there’s no way to distinguish between these outcomes until symptoms appear.
The Solution: Test Your Vitamin D Levels
If you’re supplementing vitamin D—or considering it—blood work provides the main reliable feedback. A vitamin D status test tells you what intake, sunlight, and genetics have produced in practice—not what they should produce on paper.
When to test:
➤ Baseline – If you’ve never tested, you can start now.
➤ Seasonal tracking – Late winter (March/April in the Northern Hemisphere) when levels are typically lowest; late summer (August/September) when levels peak.
➤ Adjustment phase – If you’re adjusting your intake or exploring whether low energy, sleep disruption, or cognitive fatigue could be related.
What test to order:
- Vitamin D status test (total vitamin D, including both D₂ and D₃) via your GP or primary care physician — this is the standard measure and is typically covered by insurance in most regions.
- For those who want more flexibility, the same laboratory tests can also be self-ordered without a doctor’s visit.
Interpreting results:
Standard “normal” ranges typically span 50–200 nmol/L, but recent studies on cognitive aging and sleep architecture suggest a narrower target may be more protective.
I personally aim for a range between 60-80 nmol/L based on evidence linking both deficiency and excess to poorer cognitive outcomes over time. This is narrower than the standard optimal range, but reflects what I am currently seeing in what the data suggests about long-term brain health.
The key point: avoid both extremes.
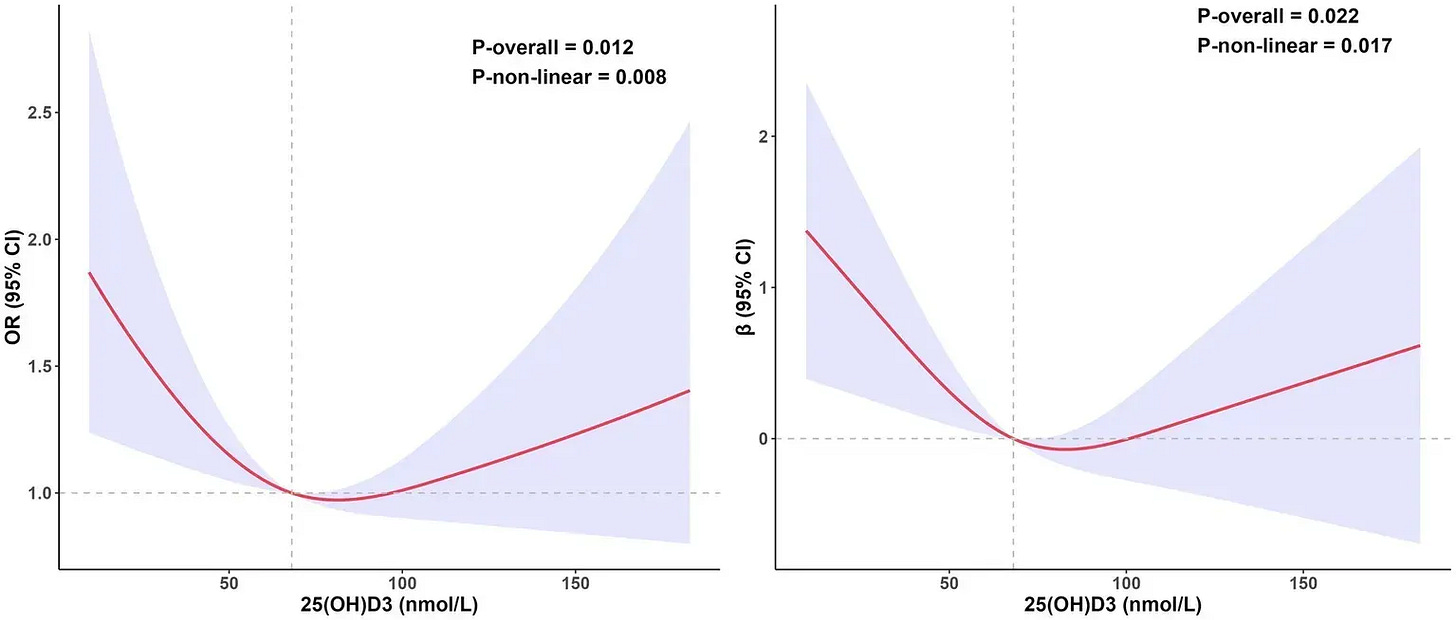
Low vitamin D is linked to poorer cognition and less stable sleep, whereas very high levels are associated with calcium imbalance, faster biological aging markers, and no added protection against Alzheimer’s disease beyond the moderate range.
If you supplement without testing, you’re essentially estimating your response rather than measuring it.
The September 2025 case shows how individual differences in metabolism can make even moderate doses unpredictable without testing.
Vitamin D Supplementation Risks: Should you supplement vitamin D regardless of what your diet looks like?
No.
Here’s why:
- Dietary intake does not predict serum levels reliably—genetic variability and individual metabolism determine your response
- Doses that seem moderate (like 4,800 IU) can cause hypercalcemia in some individuals
- Others require 20,000+ IU just to maintain adequate levels
Vitamin D is not a one-size-fits-all nutrient.
It’s a hormone precursor —a compound the body converts into the active hormone calcitriol —and it shows wide individual variation in metabolism, conversion, receptor sensitivity, and overall response.
A practical sequence might looks like this:
- Test first: A vitamin D status test provides your baseline.
- Retest after 6–8 weeks of any change; half-life and absorption vary across individuals.
- Support cofactors: Maintain adequate magnesium and vitamin K₂ intake; they balance calcium distribution.
- Adjust seasonally: Requirements fluctuate with latitude, outdoor time, and body fat percentage. A summer dose that maintains balance may overshoot in winter if lifestyle changes.
Vitamin D isn’t about more or less—it’s about knowing your range.
That’s what makes it protective
—Kat
Upgrade for personalized roadmaps—systematic implementation frameworks you can personalize to your specific biomarkers and risk factors.
References
- Wærp CM et al. Akutt nyresvikt som følge av vitamin D-forgiftning. Tidsskr Nor Lægeforen. 2025 Sep 23; 145(11).
- Zittermann A et al. Vitamin D and mortality. Curr Opin Clin Nutr Metab Care 2019.
- Autier P et al. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med 2007.
- Fu, K. (2025, March 31). Vitamin D and cognitive aging: 5 key steps to protect your brain. The Longevity Vault.
- Sizar O, Khare S, Goyal A, et al. Vitamin D Deficiency. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025
- Voltan G, Cannito M, Ferrarese M, Ceccato F, Camozzi V. Vitamin D: An Overview of Gene Regulation, Ranging from Metabolism to Genomic Effects. Genes (Basel). 2023 Aug 25;14(9):1691.
- Littlejohns TJ, Henley WE, Lang IA, Annweiler C, Beauchet O, Chaves PH, Fried L, Kestenbaum BR, Kuller LH, Langa KM, Lopez OL, Kos K, Soni M, Llewellyn DJ. Vitamin D and the risk of dementia and Alzheimer disease. Neurology. 2014 Sep 2;83(10):920-8.
- Li Y, Wang X, Yu M, Wang F, Song D, Liu M, Liang X, Liu H, Liu J, Fu S and Liu X (2025) The relationship between vitamin D levels and Alzheimer’s disease risk: insights from a centenarian study of Chinese women. Front. Nutr. 12:1628732.
- Li M, Li C, Cheng L, Lv C, Xue L, Zhang C, Bai Z, Wang X, Chen S, Guo Q, Zhao Y, Zhao H. Association of serum 25(OH)D3 and cognitive levels with biological aging in the elderly: a cross-sectional study. Front Nutr. 2025 May 12;12:1581610.
- Chen LJ, Sha S, Stocker H, Brenner H, Schöttker B. The associations of serum vitamin D status and vitamin D supplements use with all-cause dementia, Alzheimer’s disease, and vascular dementia: a UK Biobank based prospective cohort study. Am J Clin Nutr. 2024 Apr;119(4):1052-1064.
- Lönnroos E, Ylilauri M, Lamberg-Allardt C, Manson JE, Nurmi T, Uusitupa M, Voutilainen A, Hantunen S, Tuomainen TP, Virtanen JK. The Effect of Vitamin D3 Supplementation on the Incidence of Diagnosed Dementia Among Healthy Older Adults-The Finnish Vitamin D Trial. J Gerontol A Biol Sci Med Sci. 2025 Jun 10;80(7):glaf077.


