What are telomeres, and how are they associated with aging and disease?
Telomeres are protective DNA “caps” at the ends of your chromosomes. Their job is to help preserve the integrity of genetic material during cell division, when DNA has to be copied again and again. With each replication cycle, telomeres shorten a little. When telomeres become very short, cells are more likely to enter senescence (a non-dividing, pro-inflammatory state) or lose normal function.
Because of this, telomere length—especially leukocyte telomere length (measured in white blood cells)—is often used as a marker of biological aging. In large population studies, shorter leukocyte telomeres are associated with higher risk of age-related disease outcomes and earlier mortality.
So, if telomeres reflect how cellular aging, how does sleep affect how quickly those caps shorten?
Does poor sleep shorten telomere length?
A study of 434 participants examined sleep length and leukocyte telomere length. The finding was this:
- As sleep duration increased, telomere length were longer;
- As sleep duration decreased, telomere length were shorter.
🌛 Specifically: Telomeres were on average 6% shorter in those sleeping < 5 hours compared with those sleeping > 7 hours per night.
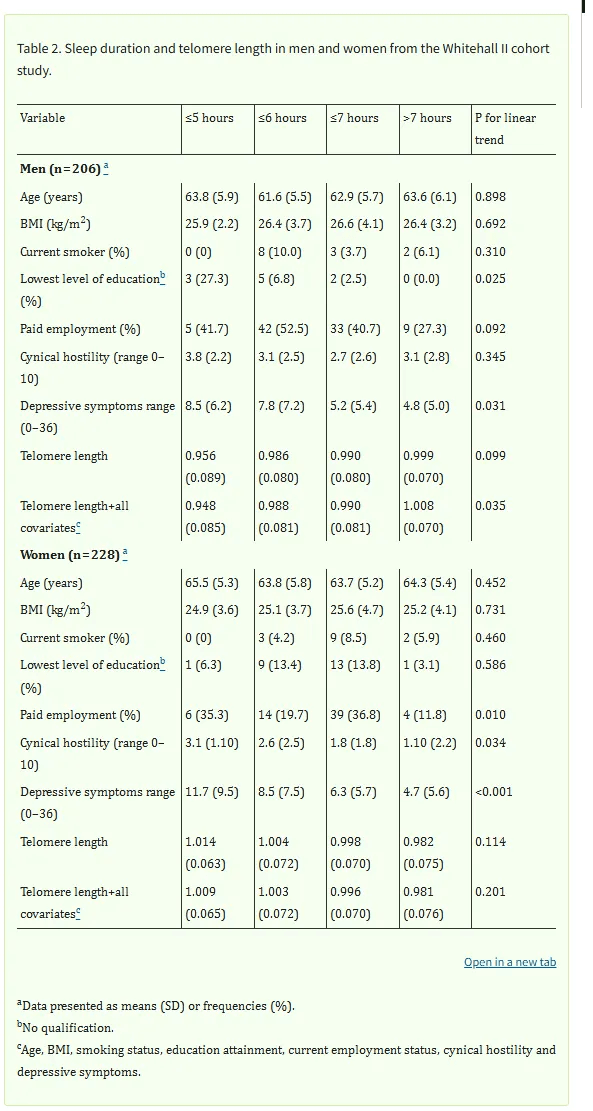
Importantly the researchers controlled for multiple potential confounding factors including:
- Age
- Body mass index (BMI)
- Smoking status
- Educational attainment
- Employment status
Inflammation as a bridge between poor sleep and shorter telomeres
Chronic, low-grade inflammation contributes to many age-related diseases
Sleep disruption is associated with elevated inflammatory activity which is part of how poor sleep drives faster cellular aging and shortens telomeres.
Here’s the logic:
- Poor sleep increases inflammatory signaling and stress physiology
- Higher inflammation can increase immune cell activation and turnover, meaning more leukocyte replication over time.
- More replication and more oxidative/inflammatory exposure can accelerate telomere shortening
Sleep in the 5–6 hour range or 3am wake ups can contribute to a chronic shift in physiology: less time in repair-dominant states, more time with elevated inflammatory tone, and more cumulative strain.
Although poor sleep has many negative effects on the body, these effects can be lessened by getting better sleep—especially in mid and late life
A practical approach is to gradually increase the frequency of ‘better’ sleep.
The sleep levers below are basic tips to help you get the external sleep disruptors out of the way.
I’m sure many of you already have most of these dialed in, but as a quick reminder, the relevant ones for midlife and older adults include:
- A consistent wake time anchors circadian rhythm and makes sleep duration easier to extend.
- If you wake frequently, prioritize interventions that reduce awakenings (temperature, alcohol, reflux).
- Early waking can respond to changes in evening light exposure, alcohol.
- Address medical disruptors. Apnea, reflux, pain are frequent medical causes of fragmented sleep in mid and late life.
Remember sleep is not only rest; it’s immune calibration and repair time.
Improving sleep length, quality and continuity can reduce inflammatory background load and help shift the body toward a slower-aging physiology
—Kat
P.S. If your sleep issues began after 40, your nervous system is doing the best it can around a new hormonal baseline. Sleep OS: Hormones helps you work on that baseline directly—without sleep medications, without more supplements, and without costly hormone workups—so you can reestablish full-night sleep and reduce the pressure sleep loss puts on brain aging and dementia risk.
👉 You can learn more about my most popular program, the Trio Hormone Sleep Recovery Course, here:
👉 Or, explore the foundational Sleep & Stress Single Hormone Sleep Recovery Course, here:
Here’s what that shift can look like:

A recent Sleep OS member who worked through the Hormone Frameworks described it this way: ‘I still get up once to use the bathroom, but I fall back asleep in seconds and I’m actually satisfied with my sleep again.
References
- Jackowska M, Hamer M, Carvalho LA, Erusalimsky JD, Butcher L, Steptoe A. Short sleep duration is associated with shorter telomere length in healthy men: findings from the Whitehall II cohort study. PLoS One. 2012;7(10):e47292.


