3AM Wake-Ups: It’s Not Just Stress
➤ “When I wake at 3AM. and see there’s barely 90 minutes until my alarm, I feel a bit of of panic. I try to focus on my breath, on my sensations, on just being, but my mind just ends up racing even more. It feels like the harder I try to breathe, the more awake I become—until the alarm finally goes off and I get out of bed.”
I hear versions of this every week—and I understand it, because I’ve been there too.
Why Breathwork and Relaxation Don’t Help with 3AM wake-ups After Midlife & Into Advanced Age
When you’ve practiced breathwork and stress management consistently but still can’t stay asleep past 5-6 hours, you’re dealing with something deeper than relaxation technique.
This pattern tends to appear in the 40s or 50s, when hormonal regulation begins to shift and the body no longer moderates stress and recovery with the same stability it once had. It can also follow long periods of sustained pressure, when both tolerance for stress and nightly restoration start to drift.
The challenge isn’t learning new ways to relax—it’s whether your body can sustain that calm state through the second half of the night.
Waking at 3AM despite skilled breathing technique isn’t just due to stress.
It’s a mismatch between the calming signal your nervous system receives and the body’s internal autonomic readiness to respond to it.
The way I explain this to clients: think of it like pressing the brakes when the brake fluid is low—the pedal works, the signal is sent, but without the internal chemistry needed to complete the response, the effect can’t fully activate—or activates too weakly.
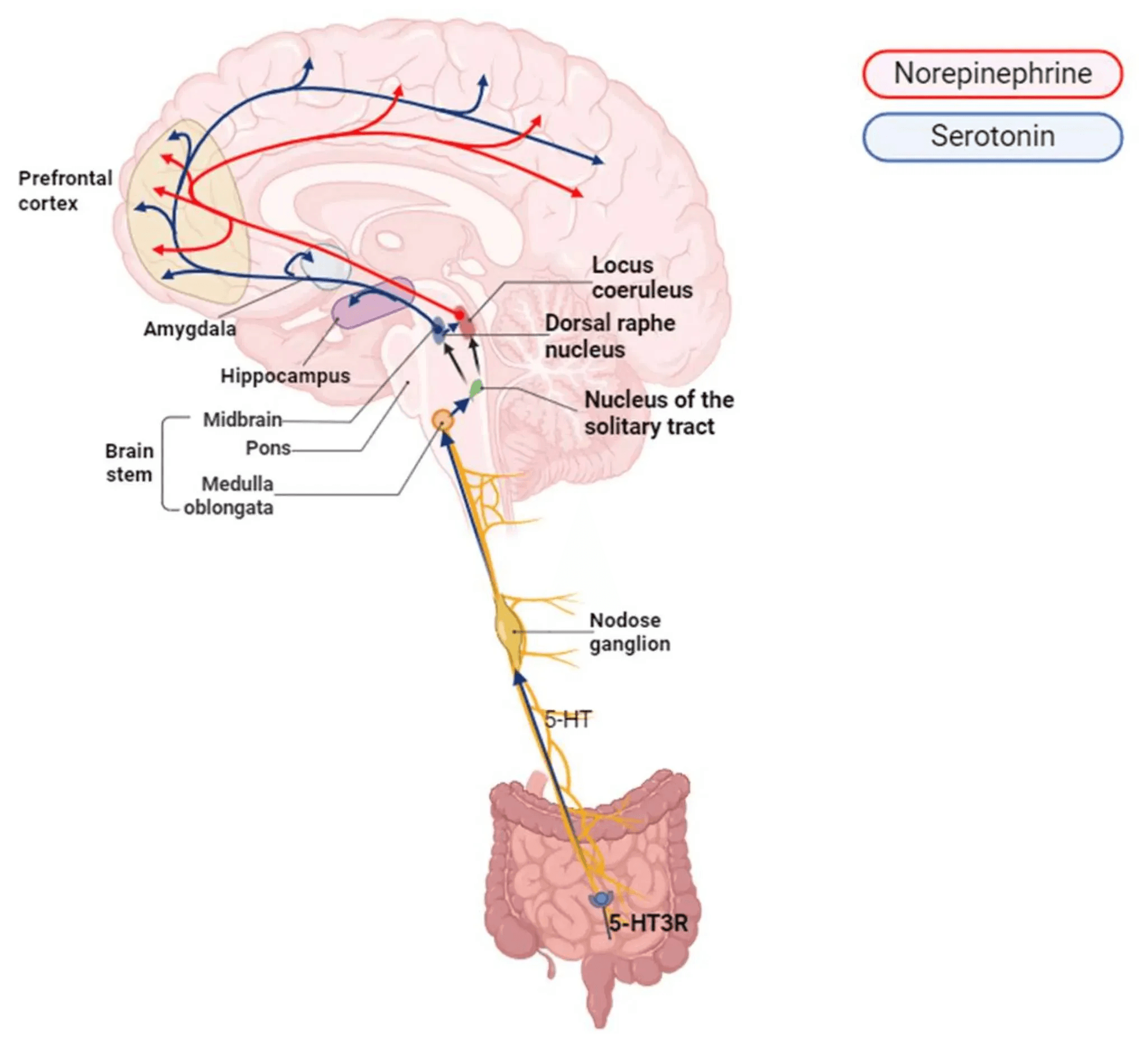
Specifically, breathwork activates the parasympathetic response through the vagus nerve, but that calming effect is influenced by hormonal status, metabolic state, and receptor-level signaling capacity.
For us who are focused on longevity, this matters beyond just feeling tired.
Fragmented sleep in the second half of the night reduces time in deeper stages that support the brain’s clearance of metabolic waste, memory processes, and cognitive resilience—functions linked to protection against cognitive decline and preserved mental sharpness with aging.
In my work with Sleep OS readers, I often see this stage arrive quietly: sleep hygiene remains strong, but recovery no longer follows. That’s the transition point where physiology needs rebuilding.
My Approach: 3 Stress-Hormone Patterns That That Fragment Sleep in Midlife and Beyond in Midlife & Into Advanced Age
For years, I’d had meditation tracks and breathing guides downloaded onto a device on my nightstand so I wouldn’t need to go online in the middle of the night.
I’d reach for it whenever I woke—or after getting up to use the bathroom—knowing I’d struggle to fall back asleep.
I’d try to calm my way back to sleep—sometimes I’d fall back asleep after 30 minutes or an hour of following the tracks, more often I’d lie awake until I needed to wake up.
What finally helped wasn’t getting better at box breathing.
It came from understanding the underlying mechanisms that govern sleep continuity after that first window—specifically what disrupts the body’s ability to sustain calm through the second half of the night.
By the way, If you’ve been following my work on hormones and sleep, you’ll know how much depth there is beneath the surface.
If you’re ready to go deeper and take a systems-based approach to improving your sleep, Sleep OS Hormones is now available as a 60-day self-guided program with dedicated systems for estrogen, progesterone, and testosterone, or bundled together for a more complete approach.
or
Here are the three factors I’ve found often associated with this pattern:
1. Hormonal Buffering Decline and Cortisol Dominance
After ~40, the hormones that once cushioned stress responses—testosterone, estrogen, and progesterone—decline or fluctuate. They normally help the brain’s master clock regulate the daily stress (cortisol) rhythm so it rises cleanly in the morning and tapers by night.
When sex hormone function declines—whether through aging, or stress itself— cortisol levels can stay higher for longer.
In addition, late-night or early-morning cortisol elevations become more common.
2. Autonomic Readiness Limits & Weaker Vagal Response
Breathing and mindfulness techniques calm the body by activating the vagus nerve, which signals safety and restores balance between the sympathetic and parasympathetic systems.
Estrogen helps modulate that balance.
It enhances parasympathetic tone and can help the vagus respond more effectively.
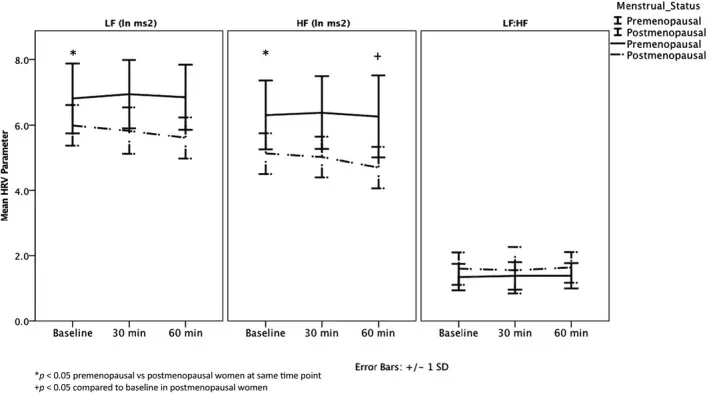
As estrogen fluctuates or declines in mid-life, overall vagal activity can weaken—meaning the same long exhale carries less physiological weight.
The vagus also functions within neurotransmitter and receptor dynamics—when these are under-supported, the body hears the cue but doesn’t fully act on it.
The result: a weaker relaxation response, even when the relaxation practice is technically flawless.
3. Temperature and Metabolic Instability in the Second Half of the Night
- Testosterone supports lean muscle and insulin sensitivity. As it drops with age or stress, glucose handling becomes less efficient. That can lead to subtle nighttime dips or rebounds in blood sugar, both of which trigger sympathetic activation—the body’s alert system.
- Estrogen influences the hypothalamic thermoregulatory centers. When levels fluctuate or fall, the thermoneutral zone narrows, making the body more reactive to small shifts in core temperature. For many individuals, this reactivity can surface in later sleep cycles—when sleep is lighter—and warmth spikes can disrupt sleep continuity.
When hormone function becomes under-supported—whether from aging or cumulative stress—heat or energy fluctuations can push the brain toward wakefulness.
See the framework we use to stabilize sleep in the second half of the night →
How Stress Signaling Rewires Sleep Architecture After 45 & Beyond
Stress itself hasn’t necessarily changed; the body’s ability to absorb it has.
Estrogen, progesterone, and testosterone once helped regulate the body’s daily rhythm of activation and recovery. They interacted with cortisol to shape the normal morning rise and evening taper of the stress response, cushioning its impact on sleep.
As hormone function declines—whether in midlife, advanced age, or through chronic stress—the body’s “shock absorbers” thin out. The same workload, emotional pressure, or everyday life demands now produces greater physiological impact.
Cortisol can rise at 2-4am—when it should be at its lowest—and triggers arousal that feels like waking “for no reason.” These mistimed cortisol peaks fragment the second half of the night, and pulls you out of deeper sleep stages.
This isn’t to say stress management tools are ineffective. It means they’re now functioning without the stress handling foundation that once made them effective.
Meditation, breathwork, or relaxation can still quiet the mind—but their effects become noticeably smaller and shorter-lived.
This is why individuals often comment familiar routines no longer deliver the same sense of recovery.
What has happened is: the underlying hormonal and stress physiology has changed.
Sleep OS Hormones is now available as a 60-day self-guided program with dedicated systems for estrogen, progesterone, and testosterone, or bundled together for a more complete approach.
Rebuilding Sleep Continuity Through Hormonal and Stress-System Support: Beyond Sleep Hygiene
Once I stopped focusing on 3AM techniques and started addressing why my body couldn’t stay asleep in the first place, my sleep became more stable.
The breakthrough didn’t come from finding different meditation tracks, trying new breathing patterns, or switching between guided body scans and sound-only recordings.
It came from understanding that breathwork sends the calming signal, but the body needs adequate hormonal support to translate that signal into sustained rest. I wasn’t waking because I couldn’t calm down—I was waking because the systems that maintain sleep continuity through the night were under-resourced.
Once I began addressing how proper hormone function support stress regulation and metabolic stability, the 3am wake-ups stopped. I no longer need the meditation tracks.
And now, my body sustains sleep on its own.
For those rebuilding this foundation, the key isn’t to collect more techniques—it’s to sequence the right physiological supports in the right order. That’s the structure behind Sleep OS: Hormones, which teaches how to stabilize the stress rhythm, temperature balance, and circadian timing so the second half of the night holds.
I still wake to use the bathroom, but I fall back asleep within seconds.
What’s interesting is that in those brief moments I’m awake, I still ruminate—thinking about what happened during the day or starting to plan tomorrow—but I can’t sustain that awareness past a few seconds before sleep takes over.
That shift—from managing middle-of-the-night wakefulness to falling back asleep almost instantly—is what became Sleep OS: Hormones, a structured, self-guided program that teaches how to support the hormonal systems that establish the foundation for continuous sleep.
P.S. If this pattern sounds familiar—whether it began in your forties or fifties, or has continued later in life despite steady sleep routines:
See who Sleep OS: Hormones was created for →
References:
- The relationship between sleep disorders and testosterone in men. Asian Journal of Andrology 16(2):p 262-265, Mar–Apr 2014. DOI: 10.4103/1008-682X.122586
- Lord C, Sekerovic Z, Carrier J. Sleep regulation and sex hormones exposure in men and women across adulthood. Pathol Biol (Paris). 2014 Oct;62(5):302-10.
- Haufe A, Leeners B. Sleep Disturbances Across a Woman’s Lifespan: What Is the Role of Reproductive Hormones? J Endocr Soc. 2023 Mar 15;7(5):bvad036.
- Schlagintweit, J., Laharnar, N., Glos, M. et al. Effects of sleep fragmentation and partial sleep restriction on heart rate variability during night. Sci Rep13, 6202 (2023).
- Irwin MR, Valladares EM, Motivala S, Thayer JF, Ehlers CL. Association between nocturnal vagal tone and sleep depth, sleep quality, and fatigue in alcohol dependence. Psychosom Med. 2006 Jan-Feb;68(1):159-66.
- Hwang, Y.K.; Oh, J.S. Interaction of the Vagus Nerve and Serotonin in the Gut–Brain Axis. *Int. J. Mol. Sci.*2025, 26, 1160.
- Haufe A, Leeners B. Sleep Disturbances Across a Woman’s Lifespan: What Is the Role of Reproductive Hormones? J Endocr Soc. 2023 Mar 15;7(5):bvad036.
- Leproult R, Ehrmann DA, Van Cauter E, Mokhlesi B. Determinants of Slow-Wave Activity in Overweight and Obese Adults: Roles of Sex, Obstructive Sleep Apnea and Testosterone Levels. Front Endocrinol (Lausanne). 2018 Jul 12;9:377.
- Stamou MI, Colling C, Dichtel LE. Adrenal aging and its effects on the stress response and immunosenescence. Maturitas. 2023 Feb;168:13-19.
- Butler KG. Relationship Between the Cortisol-Estradiol Phase Difference and Affect in Women. J Circadian Rhythms. 2018 Feb 21;16:3.
- Woods NF, Mitchell ES, Smith-Dijulio K. Cortisol levels during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Menopause. 2009 Jul-Aug;16(4):708-18.
- Scullin MK, Gao C. Dynamic Contributions of Slow Wave Sleep and REM Sleep to Cognitive Longevity. Curr Sleep Med Rep. 2018 Dec;4(4):284-293.
- Ramesh S, James MT, Holroyd-Leduc JM, Wilton SB, Sola DY, Ahmed SB. Heart rate variability as a function of menopausal status, menstrual cycle phase, and estradiol level. Physiol Rep. 2022 May;10(10):e15298.


