How to Lower LDL Cholesterol Without Statins: A Gut-First Strategy
How to turn an already strong lifestyle into lower LDL-C, reduced cardiovascular risk, and better long-term brain health by targeting gut microbes that support healthy aging.
If you have LDL-C (low-density lipoprotein cholesterol) or ApoB (apolipoprotein B, the count of atherogenic particles) higher than you want (120–200 mg/dL) there is a good chance you already have strong lifestyle habits:
- you exercise,
- you maintain reasonable body composition,
- you eat whole minimally processed foods, vegetables, healthy fats, and
- you pay reasonable attention to saturated fat.
Yet LDL-C and ApoB remain high enough that cardiovascular and brain health over the next 10–20 years are still concerns.
One under-addressed reason is that “healthy lifestyle” does not automatically create a longevity-leaning gut microbiome.
Microbial balance matters because the gut is not only a digestion site. It is an ecosystem that shapes inflammatory tone, metabolic signaling, and downstream risk patterns that touch cardiovascular health, brain resilience, and colon integrity.
Longevity-supporting Gut microbes vs inflammatory-leaning microbes is a dividing line
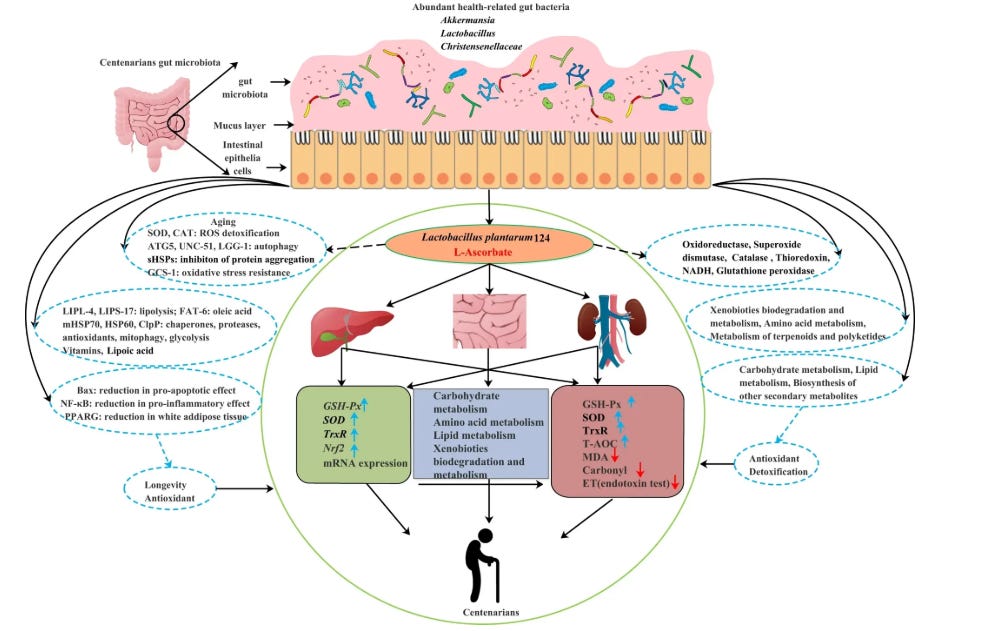
Microbiome research has accelerated in recent years and it now identifies bacterial patterns that show up more often in healthier aging populations, including centenarian cohorts. These patterns tend to share common functional traits: stronger barrier integrity, more favorable inflammatory signaling, and higher production of beneficial microbial outputs.
A few examples commonly discussed in the longevity literature:
- Akkermansia muciniphila is often associated with better metabolic health, improved insulin sensitivity, and lower inflammatory tone.
- Bifidobacterium species are linked with stronger gut barrier function, reduced frailty, and healthier immune signaling, yet tend to decline with age.
On the other side, there are microbial patterns and species more consistently associated with inflammation, barrier disruption, and metabolic dysfunction.
A few examples worth recognizing:
- Proteobacteria expansions are widely viewed as a marker of dysbiosis and inflammatory pressure.
- Bilophila wadsworthia is associated with intestinal inflammation and less favorable bile-related microbial profiles.
- Sulfate-reducing bacteria such as Desulfovibrio produce hydrogen sulfide, which in excess can irritate the gut lining and disrupt barrier integrity.
These are but a few examples of a much larger landscape.
Why “I get plenty of fiber” is too blunt for LDL-C & aging
A common response is, “I eat a lot of vegetables.”
The issue is that fiber is not one molecule. It is a label that collapses many chemically distinct structures into one word, even though microbes respond to specific structures with specific capabilities.
In other words: Microbes do not experience “fiber” as a single nutrient. They interact with a landscape of distinct carbohydrate molecules, each requiring different enzymes, supporting different groups of organisms, and producing different metabolic outputs.
A partial list of fiber families:
- Resistant starch (RS1–RS5)
- Inulin-type fructans
- Pectins (including rhamnogalacturonans)
- Beta-glucans
- Arabinoxylans and other hemicelluloses
And there are many more.
This is important because microbes are specialists. When you change the substrate environment, you change which groups have an advantage. When you keep the substrate environment narrow, you can have “fiber present” without meaningfully changing the microbial pattern that matters for cardiovascular and brain protection.
One factor to understand here is SCFAs (short-chain fatty acids)
When microbes ferment these molecules, they produce short-chain fatty acids (SCFAs) and other beneficial metabolites that influence:
- How inflammatory or anti-inflammatory the internal environment becomes
- How stable blood sugar and insulin dynamics remain over time
- How cholesterol synthesis and clearance behave at the liver
- How effectively the gut barrier protects the rest of the body
This is one reason many health conscious adults can honestly say they eat vegetables, include some fiber supplements, and still see an LDL-C profile that is not what they expect.
The question is not whether fiber exists in your life. The question is whether your overall substrate environment supports a broad set of longevity-associated populations while reducing the conditions that favor inflammatory-leaning populations.
Why psyllium often does not solve this by itself
Psyllium can be useful. It is also frequently overestimated.
The issue is not that psyllium has no effect. The issue is that, for adults who already live in a generally healthy way, psyllium is usually too narrow for what they are trying to accomplish.
Psyllium is essentially one dominant fiber structure. That means:
- It acts mainly through a narrow physical mechanism in the gut.
- It does not provide the range of raw materials required to engage the full spectrum of microbial specialists that work on the more complex fibers listed earlier.
- It does very little on its own to reshape the deeper balance between longevity-leaning microbes and inflammatory patterns.
If you already eat mostly whole foods and move regularly, a scoop of psyllium is unlikely to decide whether Proteobacteria expansions, Bilophila wadsworthia, or Desulfovibrio have abundant room to thrive, or whether Akkermansia and Bifidobacteria are consistently supported over months and years.
That is why many healthy adults end up with the same experience:
They add psyllium, notice modest change (or no change), and conclude that the microbiome angle is overrated.
More often, what happened is this: the approach was not comprehensive enough to shift microbial balance in a durable way.
This is not only about cholesterol: Microbial balance is also a colon and brain topic.
Barrier integrity and inflammatory signaling are shared roots for multiple outcomes. The same ecosystem patterns that influence cardiometabolic signaling can also shape how resilient the gut lining is over time and how much inflammatory noise is reaching the rest of the body.
If your goal is cardiovascular risk reduction and brain health protection over the next decade, it is rational to address this layer even when the rest of your lifestyle already looks strong.
Who this matters most for: adults 50+ with stubborn LDL-C
If you are 50+ and serious about health but still carry higher LDL-C or ApoB, a specific pattern tends to show up:
- Food quality, exercise, and basic risk factors are in better shape than average.
- Fiber is present in broad terms.
- There has never been a deliberate strategy to align day-to-day living with what the research shows about longevity-supporting versus inflammatory microbes.
This gap matters: Over the next decade, your arteries, brain tissue, and colon lining will exist in whatever environment the microbiome generate—either:
- More exposure to SCFAs and barrier-supportive metabolites that are associated with lower inflammation and healthier lipid profiles., or
- More exposure to endotoxins and inflammatory signals that correlate with vascular aging, metabolic disruption, and tissue-level stress.
The encouraging part is that microbial patterns are modifiable.
The challenging part is that the biology is too intricate to adjust a few habits and expect the gut to consistently behave like what we observe in healthier aging cohorts.
The missing piece is a research-grounded way that translates the science on specific microbes and fiber families into something you can apply week after week without designing it from scratch.
The 5-Phase Gut-LDL-C Blueprint for Lower Cholesterol + Reduced Cardiovascular Risk: A strategy to support longevity-leaning microbes & lower LDL-C
The 5-Phase Gut-LDL-C Blueprint helps you support longevity-associated microbes and reduce the conditions that favor inflammatory-leaning populations, using a phased, week-by-week approach over a personalized timeline.
It is for adults whose LDL-C or ApoB remain elevated despite strong habits, and who want a practical way to:
- Support microbial communities that appear more often in healthier, longer-lived populations
- Crowd out inflammatory-leaning microbial patterns
- Do this in a phased fashion across several weeks so adaptation feels realistic and does not depend on constant tracking or complex planning
Inside the Blueprint, you are not asked to reverse-engineer the literature on Akkermansia, Bifidobacteria, Proteobacteria, Bilophila, Desulfovibrio, etc, and what they respond to.
That work is already done and organized into a stepwise approach you can follow.
Inside, you get:
- A longevity microbiome reference layer that explains which populations show up more often in healthier aging patterns
- A microbial displacement lens that clarifies which inflammatory-leaning patterns you are trying to crowd out
- A phased plan with personalized progression options that supports longevity-associated microbes and displaces inflammatory-leaning patterns week by week, with adaptation guidance so it is sustainable for your baseline and your adaptation.
- A references library (70+ references from 1990-2025) for deeper reading and clinician-level conversations
If you have already handled the basics and your LDL-C still has not responded, this is a step-by-step strategy to align your lifestyle with what the latest evidence suggests about microbiome patterns that support lower LDL-C, reduced cardiovascular risk, and better protection for brain and colon health as you age.
You can access The 5-Phase Gut-LDL-C Blueprint for Lower Cholesterol + Reduced Cardiovascular here:
It gives you the same structured gut–bile–LDL approach I would normally work through across multiple sessions, but in a format you can implement at your own pace.
You shouldn’t have to treat statins as the only “serious” next step when lifestyle hasn’t moved your numbers; with The 5-Phase Gut-LDL-C Blueprint, you won’t.
This is accessed through a private link to the Dashboard (shown below) you receive, so you’re getting a structured & live digital resource—not a static PDF file:
All my digital solutions are updated regularly: The 5-Phase Gut-LDL-C Blueprint (based on 70+ peer reviewed articles) was just updated to incorporate the latest data on longevity-promoting microbes and how to support them. All existing owners and Vault Insiders automatically have access to the new edition, and that access remains active even as new editions are released at higher investment levels.

References
- Strong JP et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA. 1999 Feb 24;281(8):727-35.
- Díaz Perdigones CM et al. Taxonomic and functional characteristics of the gut microbiota in obesity: a systematic review. Endocrinol Diabetes Nutr (Engl Ed). 2025 Nov;72(9):501624.
- Singh P et al. Implications of the gut microbiome in cardiovascular diseases: association of gut microbiome with cardiovascular diseases, therapeutic interventions and multi-omics approach for precision medicine. Medical Microbiology. 2023.
- Wu L et al. Gut microbiota as an antioxidant system in centenarians associated with high antioxidant activities of gut-resident Lactobacillus. npj Biofilms Microbiomes. 2022;8:102.
- Benjamin EJ et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137(12):e67-e492.
- Cui X et al. Metagenomic and metabolomic analyses unveil dysbiosis of gut microbiota in chronic heart failure patients. Sci Rep. 2018 Jan 12;8(1):635.
- Wang Z et al. Non-lethal inhibition of gut microbial trimethylamine production for the treatment of atherosclerosis. Cell. 2015 Dec 17;163(7):1585-95.
- Poland JC et al. Bile acids, their receptors, and the gut microbiota. Physiology (Bethesda). 2021 Jul 1;36(4):235-245.
- Razavi AC et al. High-density lipoprotein cholesterol in atherosclerotic cardiovascular disease risk assessment: exploring and explaining the U-shaped curve. Curr Cardiol Rep. 2023 Dec;25(12):1725-1733.
- Zhou Z et al. Low-density-lipoprotein cholesterol and mortality outcomes among healthy older adults: a post hoc analysis of ASPREE trial. J Gerontol A Biol Sci Med Sci. 2024 Apr 1;79(4):glad268.
- De Oliveira-Gomes D et al. Apolipoprotein B: bridging the gap between evidence and clinical practice. Circulation. 2024 Jul 2;150(1):62-79.
- Ghavami A et al. Soluble fiber supplementation and serum lipid profile: a systematic review and dose-response meta-analysis of randomized controlled trials. Adv Nutr. 2023 May;14(3):465-474.
- Dahl WJ et al. Position of the Academy of Nutrition and Dietetics: health implications of dietary fiber. J Acad Nutr Diet. 2015 Nov;115(11):1861-70.
- Svilaas T et al. High levels of lipoprotein(a) – assessment and treatment. Tidsskr Nor Laegeforen. 2022 Dec 16;142(1).
- Gaba P et al. Association between achieved low-density lipoprotein cholesterol levels and long-term cardiovascular and safety outcomes: an analysis of FOURIER-OLE. Circulation. 2023 Apr 18;147(16):1192-1203.
- Grundy SM et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary. J Am Coll Cardiol. 2019 Jun 25;73(24):3168-3209.
- Cholesterol Treatment Trialists’ (CTT) Collaboration et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010 Nov 13;376(9753):1670-81.
- Ference BA et al. Effect of long-term exposure to lower low-density lipoprotein cholesterol beginning early in life on the risk of coronary heart disease: a Mendelian randomization analysis. J Am Coll Cardiol. 2012 Dec 25;60(25):2631-9.
- Sabatine MS et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017 May 4;376(18):1713-1722.
- Schwartz GG et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018 Nov 29;379(22):2097-2107.
- Zhou Z et al. Low-density-lipoprotein cholesterol and mortality outcomes among healthy older adults: a post hoc analysis of ASPREE trial. J Gerontol A Biol Sci Med Sci. 2024 Apr 1;79(4):glad268.
- Chwal BC et al. On-target low-density lipoprotein cholesterol in adults with diabetes not at high cardiovascular disease risk predicts greater mortality, independent of early deaths or frailty. J Clin Med. 2024 Dec 16;13(24):7667.
- Madsen CM et al. Extreme high high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J. 2017 Aug 21;38(32):2478-2486.
- Jacobson TA et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: Part 2. J Clin Lipidol. 2015 Nov–Dec;9(6 Suppl):S1-122.e1.
- Gidding SS et al. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Risk Score in young adults predicts coronary artery and abdominal aorta calcium in middle age: the CARDIA Study. Circulation. 2016 Jan 12;133(2):139-46.
- Sniderman AD et al. Apolipoprotein B particles and cardiovascular disease: a narrative review. JAMA Cardiol. 2019 Dec 1;4(12):1287-1295.
- Giugliano RP, et ak; FOURIER Investigators. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet. 2017 Oct 28;390(10106):1962-1971.