A member recently asked me something that captures what so many health-conscious adults wonder but don’t always say out loud:
“I sleep 5–6 hours, wake up feeling ‘fine’ once the coffee kicks in, and I still get through my day. Lately though, I need more caffeine just to stay focused. If I’m functioning on 5–6 hours, how big a deal can my sleep really be?”
I’ve asked myself this same question more times than I can count.
And it’s a reasonable question: A lot of smart, health-aware adults work, drive, make decisions, even exercise on 5–6 hours. Life mostly runs.
So if everything still functions — how urgent can sleep really be?
Here’s what I wish someone had explained to me years earlier:
What “feeling fine” actually requires: reliance on alertness chemistry to keep you going.
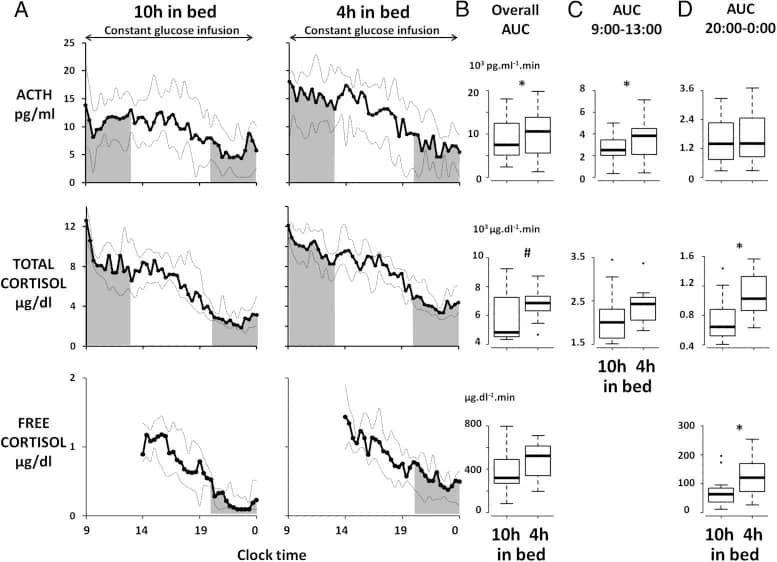
Specifically: stress hormones — cortisol, adrenaline, and their downstream chemistry — are picking up the slack. They’re keeping you alert, focused, and moving through your day when your sleep didn’t provide the restoration to do it naturally.
It’s an adaptive response. Your body is doing what it evolved to do when recovery is incomplete: mobilize resources to keep you operational.
The problem is what that mobilization costs when it becomes the norm rather than the exception.
Elevated stress chemistry doesn’t just keep you awake.
It moves blood pressure upward. It makes blood sugar harder to stabilize. It increases appetite and shifts where your body stores fat. It shortens your fuse emotionally, even when you don’t notice it consciously.
The more often your body runs on stress chemistry instead of genuine restoration, the more your baseline shifts. “Wired” starts to feel like “normal.” You lose the reference point for what true recovery feels like.
That same high-alert state is also what makes it harder for your brain and body to downshift fully at night. In other words, the same pattern that lets you “power through” today can make the next sleep episode more easily disrupted,
For years, many of us were reassured that if we can handle our day, stay on top of our schedule, and still make it to the gym, your sleep is “good enough.”
In short appointments, the focus often lands on whether anything looks wrong on basic labs — not on what years of 5–6 hours of sleep are doing in the background. When someone mentions waking at 3–4 a.m., the response is often a shrug, a refill, a suggestion to manage stress better, or “that’s common as we get older,” rather than a deeper look at what keeps that pattern in place.
At the same time, we’re surrounded by messages selling us ways to push through another day on less sleep — new coffees, adaptogens, and ‘energy formulas.’
The idea underneath all of it: you can out-supplement or out-caffeinate fatigue and still call it health. We’re encouraged to celebrate being wired and productive, even when that buzz is mostly stress hormones doing overtime.
Very few of these messages pause to ask what it means when your body needs that much stimulation just to feel fine.
Between quick reassurances that “you’re fine if you can function” and a culture that sells more ways to feel wired, it’s easy to miss that your daytime “fine” is built on stress chemistry — and that stress chemistry is not a substitute for the restoration that protects your brain, metabolic health, and independence over the next 10–20 years.
If you’ve spent a long time in that mode, it can be surprisingly challenging to remember what a good sleep feels like.
People who gradually improve sleep often describe a shift that is more about texture than intensity:
- Focus feels more even
- Routine stressors feel easier to absorb
- Energy no longer depends on caffeine
If you have spent a long time running on compensation, it is possible you have never experienced that state for more than a few days at a time. That makes it very hard to use your current “fine” as a benchmark —its also why “I can function” is a poor proxy for “my sleep is supporting my longevity and vitality.”
What changes once you recognize that “feeling fine” is stress hormones doing the heavy lifting?
—it becomes harder to treat your current sleep pattern as a low priority.
You don’t have to accept the idea that as long as you can get through the day, your sleep is good enough.
You can decide that how your body gets you through the day matters — not just whether it can.
And that decision is yours to make, regardless of what anyone else has told you about what’s “normal” for your age or stage of life.
Warmly,
Kat
P.S. Now you have another lens — one that empowers you to start treating your sleep as a core part of how you steer your health going forward, on your terms, with better information, and with a longer horizon than “I got through today.”
If you want to hold the steering wheel on your own physiology, with rigorous, evidence-based tools that support independent decisions instead of ongoing dependence on the wellness economy, you can explore my longevity tools and my flagship sleep recovery program.