Do you ever find yourself thinking: “I’m 52, I wake up around 3–4 a.m., and I function. Maybe I just need less sleep now.”
You may have started noticing sleep changes in your 40s or 50s. By now, you may have been getting no more than 5–6 hours for years, if not decades.
On top of that, you keep hearing from friends, headlines, and perhaps even clinicians that this is “just what happens with age.” Over time, it can start to feel as if your body needs less sleep and that this lighter pattern is your new normal.
But that’s not what’s happening.
The National Institute on Aging refers to the belief that “people need less sleep as they age” as a myth and still points adults to 7–9 hours, with those 65+ recommended at 7–8 hours of sleep each night.
Yale Medicine similarly notes: the recommended sleep ranges for adults in their 20s, 40s, 60s, and 70s are almost identical.
So you’re in a strange position:
- Your lived reality is 5–6 hours with a 3–5 a.m. wake-up that feels bothersome but normal for your age.
- Yet, the official guidance still says: you would do better, across years, with 7–8 hours.
Here’s the encouraging bit: although this pattern is common—it’s changeable.
Those same guidelines that still point 65- and 70-year-olds toward 7–8 hours are a reminder that your capacity for deeper, more continuous sleep is still on the table, regardless of your age.
So a more helpful question becomes: what is the quality of life and health impact to live at 5–6 hours of sleep over many years—and why has it been so hard to move beyond that ceiling?
Let’s start with how that pattern shows up in everyday life.
A slow gradual pinch on daily life: Short sleep → worse mood + higher BMI
If you’re getting up, working, and generally keeping life running, it can feel rational to push the sleep problem down the list. After all, 5-6 hours doesn’t usually show up as “I can’t function.” Instead, it usually shows up as small changes that make each day a little harder to run:
- Your emotional range tightens. Little stressors hit harder. Patience gets thinner.
- Your body composition nudges in the wrong direction even when your habits haven’t changed.
- Your appetite and cravings get louder at the wrong times.
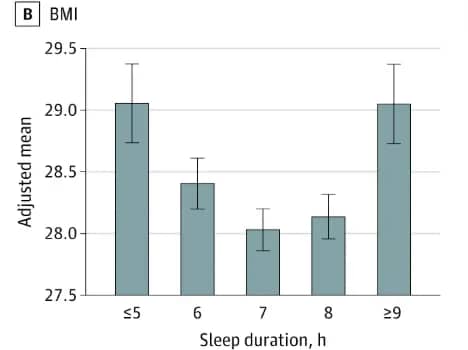
For example, in 2021, Stanford University’s Departments of Neurology and Psychiatry collaborated on a study of 4,417 cognitively healthy adults ages 65–85, comparing ~7–8 hours of sleep VS. ~5–6 hours. The shorter-sleep group had:
- Higher depression
- Higher body mass index
These are the kinds of day-to-day changes that feel subtle in the moment, then accumulate—and add friction to everything else you’re trying to do for your health.
Now, the long-horizon piece.
Poor sleep → higher Alzheimer’s amyloid buildup in the brain
The same Stanford study of cognitively healthy older adults also looked at sleep duration and matched it to brain scans that measure amyloid-β—the protein that accumulates in Alzheimer’s disease. They found:
- those who slept 5–6 hours had more amyloid-β in their brains vs. those who slept 7–8 hours
- the researchers took age, education level, and APOE genotype (a genetic risk factor for Alzheimer’s) into account, and the pattern still showed up.
So when your body adapts to 5–6 hours sleep, there is a impact to your brain and to how your days feel now.
So, why it has been so hard to move beyond that 5-6 hour sleep ceiling? (Here are 4 reasons why)
You’ve been doing much of the things health-conscious adults are told are proactive: supplements, upgrades, apps—because the wellness ecosystem rewards that proactivity by steering you toward one main path: buying more fixes.
The issue is that most of what the wellness ecosystem offers doesn’t reach the part of your physiology that keeps you asleep.
1. Narrow sleep fixes that don’t fit the complexity of your midlife + later-life physiology
As one example, melatonin can make you feel more drowsy at the start of the sleep.
But the challenge you have isn’t falling asleep—it’s staying asleep. This is why people I work with so often describe some version of “It takes the edge off, but I still wake up at 3–4 a.m.”
Benadryl, or PM combinations often get pulled in as a stronger version of the same plan.
But, your body is running a complex program underneath. This means that tools that help you fall asleep at 10 p.m. are not the right tools to help you stay asleep.
In my work, we use melatonin strategically when it’s appropriate—but we don’t rely on it to address a 3–5 a.m. wake-up.
The same applies to cooling tech: The sleep cooling market keeps growing—cooling mattresses, pads, sheets, etc. And yet, individuals I work with tell me they’ve tried them and are still waking up hot.
This is how I explain it to them: the heat isn’t coming from your environment. It’s coming from inside—a core temperature surge your body generates when certain hormonal processes are disrupted / under-supported.
2. Sleep monitors watch you, but don’t teach you
Trackers and wearables reduce physiology to a few metrics (HRV, resting heart rate, “recovery”) that don’t capture the full complexity of sleep maintenance and late-sleep disruption.
You’re also nudged toward one-size advice (“improve your score”) instead of a way to ask targeted questions about your sleep patterns—questions that account for your age, health status, and the specific way your sleep breaks down.
So, the Apple Watch, rings, and other trackers are impressive pieces of engineering—and when we’re using them, they can feel like progress.
(And, I understand why. I spent years checking my deep-sleep minutes every morning—sometimes, I would even check it in the middle of the night to see ‘how my sleep was going.’)
What I eventually realized, and what I hear from my clients as well, is the same growing frustration: much of the time, they tell us little more than what we already sense—that we had a poor night’s sleep.
We get plenty of color-coded feedback. What we don’t get is a map that links our sleep pattern to health context we can act on—or a framework for asking better questions about our sleep physiology.
3. Sleep gummies that create a higher dose next month—not a more confident you
Over time, this dynamic compounds the original challenge: The supplement that worked at first requires a higher dose a year later. The tracker that was supposed to bring clarity becomes its own source of anxiety.
Instead of giving you more confidence in reading and supporting your sleep physiology, the wellness cycle pulls you into investing more energy managing health management itself—all the while the fundamental question stays unanswered:
What is my body doing at 3 a.m., and how can I support its capacity to sleep more intelligently?
4. Renting temporary sleep fixes month after month without building sleep capacity
The wellness economy offers convenience—but at the cost of your agency: you spend ongoing mental and financial resources choosing brands, tracking, subscribing—without gaining understanding.
They treat your sleep as a consumer problem (“optimize your setup”) rather than a physiology problem—your body’s own capacity to stay asleep—something that you can rebuild.
And that core question almost never gets raised—because the wellness economy wants you focused on products.
Underneath, it’s a business model that relies on repeat purchases, upgrades, and ongoing dependence on proprietary scoring.
For you, the cost isn’t just financial.
It’s the years spent cycling through products without arriving anywhere—while the core issue, your body’s own foundational evolutionary capacity to sleep, remains unaddressed.
You need more than another wellness sleep product: When I see a client who’s been living with a 5–6 hour ceiling for years—sometimes decades— another wellness product usually isn’t what changes the trajectory.
What changes things is a framework that answers the question: what is your body doing at 3 a.m., and how can you support it—in a sequence that matches the complexity of your physiology,
Inside Sleep OS, that sequence is built into the Testosterone–Sleep, Stress & Energy Recovery Suite (60-day sequence), guided by the Testosterone–Sleep Pattern & Pathway Navigator.
(Testosterone is the example here—same components exist for estrogen and progesterone, same depth, same structure, specific to that hormone.)
A lifelong longevity asset
You keep Sleep OS as a lifelong longevity asset in your toolkit — instead of renting a solution that disappears the moment you stop paying a monthly subscription or coaching fee. It’s searchable and usable from any device,—so you use it as a living sleep reference you can come back to whenever you want.
Within that, the Sleep OS, Testosterone Function & Sleep Atlas stays evergreen as your pattern evolves. It gives you a testosterone–sleep architecture foundation, connecting testosterone to circadian timing, stress buffering, growth hormone, and energy balance—so you see how broadly it shapes sleep and recovery, and how many influential factors you can still address at any age—without relying on prescriptions.
Scope & depth that matches your physiology & the problem you’re living
Sleep disruption is not a one-metric problem.
With Sleep OS, you implement a rigorous, evidence-based, multi-layered strategy that addresses the complexity of midlife+ physiology and your changing hormonal landscape—not a simplified version designed for mass appeal—and without turning your sleep into a perpetual self-tracking project.
Inside that approach, the Testosterone Function & Sleep Atlas helps you translate science into decisions you can act on:
- You identify your highest-leverage vulnerability drivers across 10+ testosterone disruption factors beyond age—so you can prioritize what to address first.
- You connect what testosterone function needs across production, transport, receptor sensitivity, and clearance (based on 170+ peer-reviewed studies) to concrete actions—so you feel confident you’re following a rigorous, evidence-informed path to better sleep.
Less overwhelm, more confidence
Instead of trying to fit yourself into one more one-size-fits-all plan, you begin by personalizing the solution to you—your baseline, your constraints, your season of life, your sleep patterns.
You use the Testosterone–Sleep Pattern & Pathway Navigator to map your implementation path, susceptibility profile, and time realities in one place—so you see which path you’re on, how to sequence it, and when to revisit.
The overwhelm of conflicting advice gives way to a navigable roadmap that rebuilds your body’s own capacity to sleep, in a sequence that respects both your time and your physiology.
Most importantly, you build sleep capacity in your own body instead of health dependency.
— so you’re less reliant on the wellness cycle that keeps you buying fixes instead of acting on what your sleep needs.
The question—what is my body doing, and how can I support it?—finally gets answered.
And the answer stays with you.
If you have recognized your own pattern in the 5–6 hour ceiling since midlife and persisted since then, you can learn more about how Sleep OS: Hormones works here.
Warmly,
Kat
P.S. If you’re ready to treat your sleep as a core part of how you steer your health in the coming years—on your terms, with better information, so you can wake with energy to pursue your passions & hobbies, enjoy your life, and show up fully for what matters—you can explore the different Sleep OS sleep solutions here.