Your Sleep Study Came Back Normal—But Your Sleep Still Isn’t.
“I finally got referred to a sleep clinic after years of terrible sleep. After the overnight test, they said my results showed ‘mild sleep fragmentation’ but nothing that met their criteria for concern. I left with a printout of sleep hygiene tips I’d been following for years. Nearly 10 months + $3,000 later, I’m still waking up at 3 a.m.”
The sleep study had worked exactly as designed
But the core problem—the repeated 3 a.m. wake-ups—was still there.
This disconnect between “normal” results and persistent poor sleep happens more often than most people realize.
So does this mean you shouldn’t get a sleep study?
By the way, If you’ve been following my work on hormones and sleep, you’ll know how much depth there is beneath the surface.
If you’re ready to go deeper and take a systems-based approach to improving your sleep, Sleep OS Hormones is now available as a 60-day self-guided program with dedicated systems for estrogen, progesterone, and testosterone, or bundled together for a more complete approach.
or
Not necessarily.
But understanding what sleep clinics can help you fix—and more importantly, what they can’t—can save you thousands of dollars and years of frustration.
Here’s what we will discuss:
- what sleep clinics measure well, what they consistently miss,
- how to decide whether a sleep clinic test, a home test, or different approach makes sense for your situation—and—
- most importantly—what to investigate when your results come back normal but sleep problems persist.
Let’s get started.
Section 1: What Sleep Clinics Can and Cannot Solve
What Sleep Clinics Excel At Measuring
Overnight polysomnography captures a set of physiological signals designed to detect specific categories of sleep disruption.
These include: airflow via nasal cannula, respiratory effort through chest and abdominal belts, oxygen saturation by fingertip sensor, EEG to score sleep stages, EOG for eye movements, EMG for muscle tone, and additional channels for snoring and body position.
These inputs make it possible to detect:
- Obstructive or central apneas
- Hypopneas and partial flow limitation
- Arousals tied to respiratory effort (including RERA events)
- REM-specific airway collapse
- Positional breathing restriction
- Periodic limb movements associated with arousals
This combination allows sleep clinics to identify and quantify breathing-related sleep fragmentation and limb-driven arousals with a high degree of resolution.
In particular, studies can reveal flow-limited breathing that does not meet the apnea–hypopnea threshold but still disrupts sleep architecture, often seen in upper airway resistance syndrome (UARS). Similarly, PLMS (periodic limb movement syndrome) scoring can highlight repetitive leg movements that lead to subcortical arousals or full awakenings.
The purpose of the lab night is not to provide a holistic assessment of sleep quality.
Rather, it is to detect and document physiological events that fragment sleep in quantifiable ways, primarily for documentation that supports device-based sleep treatment options (e.g., CPAP).
What Sleep Clinics Usually Can’t Solve
When sleep disruption is driven by rhythm instability, conditioned wakefulness, or low-arousal fragmentation, these same measurement tools often fail to produce actionable findings.
Overnight sleep clinic testing typically is not designed to assess:
- Internal circadian phase (e.g., melatonin rhythm, core body temperature minimum)
- Wakefulness maintained without external disruption
- Sub-threshold micro-arousals that don’t meet the scoring criteria for an arousal index
- Learned hyperarousal patterns (e.g., waking at the same time each night despite no respiratory event)
- Variability across nights
The structure of the study itself creates limitations.
Two factors contribute to this gap:
- First-night effect is a well-documented phenomenon in which REM latency, density, and overall sleep architecture are altered by the novelty of the environment and the presence of monitoring equipment.
- In addition, many of the usual contributors to disrupted sleep—partner movement, environmental noise, temperature fluctuation—are absent or different, making the captured data less representative of your typical sleep environment.
The result is that many people receive a report that reads mostly normal despite continued real-world issues with sleep. In those cases, the lab succeeded at its task: it ruled out clinically defined breathing and movement disorders.
But it did not—and was never intended to—identify the type of non-apneic, non-movement fragmentation that occurs in circadian, hormonal, environmental or autonomic mismatch.
Given these limitations, it might seem tempting to skip sleep clinic testing altogether.
But before exploring alternative approaches, it’s worth ensuring that breathing-related sleep disruption isn’t what you’re dealing with—since untreated sleep apnea progressively affects overall health.
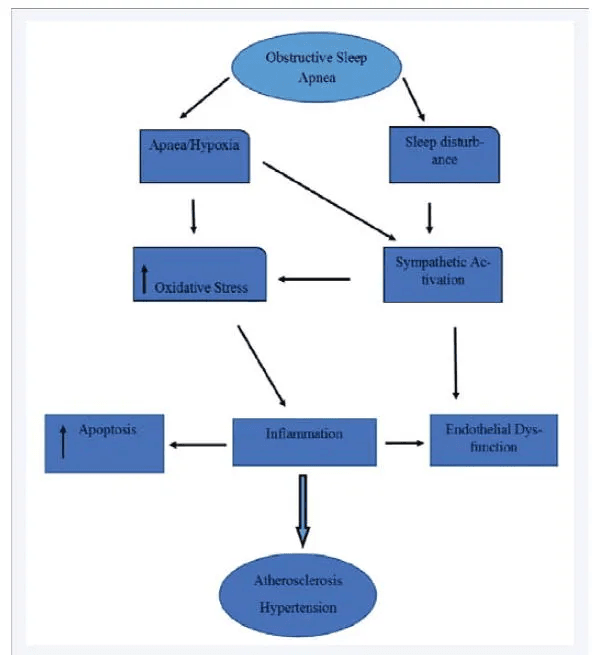
How sleep apnea/hypoxia contributes to cardiovascular disease
Additionally, airway instability can involve anatomical factors—that require professional evaluation and often prescription devices oral appliances that need proper fitting and titration.
Section 2: How to Recognize Sleep Apnea Patterns
Sleep apnea is one of the most studied and treatable causes of sleep disruption, yet many people with poor sleep haven’t considered whether breathing issues might be involved.
If you haven’t explored this possibility—or if you’re unsure whether your patterns point toward airway instability—it’s worth understanding what breathing-related sleep disruption looks like. This can help you decide whether sleep clinic testing makes sense as a first step
That begins with understanding what airway-based disruption can looks like, both subjectively and physiologically.
What Sleep Apnea Can Look Like
When sleep is fragmented by unstable breathing, the architecture tends to follow a specific pattern. These disruptions most often present as multiple brief arousals rather than one long awakening and often occurring without conscious awareness.
While the individual events may go unnoticed, their downstream effects often do not.
The result is sleep that feels shallow or unrefreshing, even when total sleep time appears sufficient. Morning symptoms may include elevated blood pressure, dry mouth, headache, or multiple trips to the bathroom.
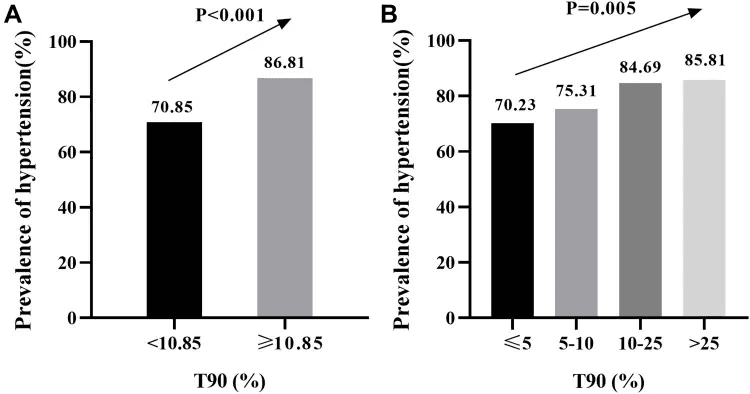
Sleep apnea patients with more severe oxygen drops show higher rates of hypertension. As time spent below 90% oxygen saturation (T90) increases from light to severe hypoxia, blood pressure problems become more common.
T90 categories: Light ≤5%, Mild 5-10%, Moderate 10-25%, Severe >25% of sleep time below 90% oxygen saturation.
At the root of these interruptions is typically a disruption in airflow or ventilatory control. Partial or complete airway obstruction leads to changes in oxygen saturation, increased respiratory effort, or elevated sympathetic tone. These events trigger micro-arousals, restoring airway patency but preventing continuous, restorative sleep.
In some cases, the arousals are audible—snoring, choking, or gasping. But many occur without noise or external signs. And, the absence of reported breathing events doesn’t reliably exclude a breathing-related cause.
However, some patterns are less commonly linked to breathing issues. For example, if your only challenge is falling asleep at the beginning of the night—and you stay asleep through the night, waking fully refreshed—airway instability is less likely to be the primary issue.
That said, breathing-related sleep disruption can be subtle and variable. Many apneas don’t produce obvious symptoms, and even unrefreshing sleep without dramatic signs may still point toward airway instability.
Sleep studies are designed to detect these patterns and can identify: ▪️ Obstructive apneas and hypopneas ▪️ Respiratory effort–related arousals (RERAs) ▪️ Stage- or position-specific airway collapse (e.g., REM-related, supine-only) ▪️ Central sleep apnea driven by ventilatory control instability
If you recognize multiple brief awakenings, morning symptoms like dry mouth or headaches, or unrefreshing sleep despite adequate time in bed—consider pursuing apnea screening through home testing or a sleep clinic evaluation.
Can Sleep Apnea Appear Suddenly?
Most forms of sleep apnea—especially obstructive sleep apnea (OSA)—develop gradually.
It’s common for the airway to become less stable over time, with symptoms like snoring, shallow breathing, or unrefreshing sleep building slowly and going unnoticed for years.
But in some cases, the pattern can shift more abruptly.
What feels like “sudden onset” is often crossing a threshold—where previously manageable airway instability becomes disruptive enough to fragment sleep.
That threshold can be tipped by changes in airway tone, ventilatory control, or arousal threshold. For example:
- Rapid weight gain
- Nasal blockage from allergies, illness, or structural issues
- New sedating medications
- Hormonal transitions, including menopause, which increases airway instability and may present with subtler symptoms
- Thyroid dysfunction or changes in autonomic regulation
- Cardiac or neurological shifts
In these cases, previously mild symptoms may become more pronounced—or new patterns may emerge.
In another scenario, central sleep apnea, which arises from instability in the brain’s respiratory rhythm generator, can appear more suddenly than obstructive forms. It often emerges alongside other health changes—particularly cardiac, neurological, or respiratory control issues—and may not involve snoring or obvious obstruction.
So while most apnea patterns evolve over time, a noticeable shift in sleep quality—especially when paired with any of these factors—can signal that the airway or control system might benefit from evaluation.
Whether your sleep disruption developed gradually or appeared suddenly, there are ways to gather preliminary clues about breathing-related patterns.
Note that some sleep clinics now offer home sleep testing as a first step anyway.
Section 3. Detecting Sleep Breathing Issues at Home & Some Alternative Home Assessment Methods
Before deciding whether to pursue testing, it’s worth understanding what you can—and cannot—learn from observations at home. Many people start here, gathering clues from partners or their own awareness of sleep patterns.
What Partners and You Can Notice About Breathing During Sleep
If you share a bed, your partner may notice breathing irregularities you’re unaware of—loud snoring, breathing pauses, gasping sounds, or physical restlessness like frequent position changes or appearing to struggle with breathing.
Even sleeping alone, you may notice some patterns. In addition to dry mouth, waking up with a racing heart or feeling like you’ve been holding your breath can point toward breathing disruption during sleep.
These observations provide useful starting points for recognizing patterns.
However, many breathing disruptions involve only subtle reductions in airflow that cause mild hypoxia (reduced oxygen levels), triggering brief brain arousals to restore normal breathing without creating obvious external signs. Upper airway resistance, for example, increases breathing effort without full obstruction—your body works harder to move air through a partially narrowed airway, that fragments sleep without producing audible sounds.
Additionally, some breathing events occur only during specific sleep stages (like REM) or body positions, making them intermittent and easily missed during casual observation.
This is where monitoring tools can help capture patterns that escape human detection.
Recording Apps, Pulse Oximeters, and Home Sleep Tests for Breathing Assessment
Moving beyond simple observation, several tools can capture breathing patterns that might otherwise go unnoticed:
- Audio Recording: Simple voice recording apps can capture breathing patterns, snoring intensity, and irregular respiratory rhythms that might otherwise go unnoticed. Record several nights to identify consistent patterns.
- Pulse Oximetry: Basic pulse oximeters can track blood oxygen levels and heart rate fluctuations throughout the night. Repeated dips and rebounds in oxygen saturation can indicate breathing disruptions, even when no one hears them happening.
- Home Sleep Testing: These tests measure airflow, breathing effort, blood oxygen, and heart rate trends while you sleep in your familiar environment. They provide objective data about respiratory events and can quantify the severity of breathing-related sleep disruption.
If your home observations suggest patterns of disrupted breathing, clinical evaluation becomes the logical next step.
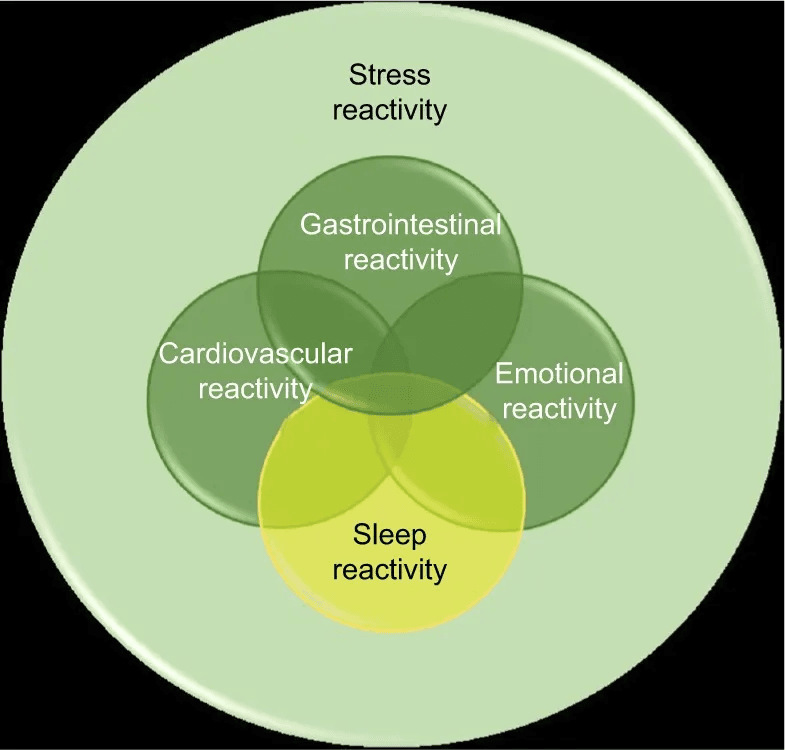
Relationships between sleep reactivity and the other components of stress reactivity.
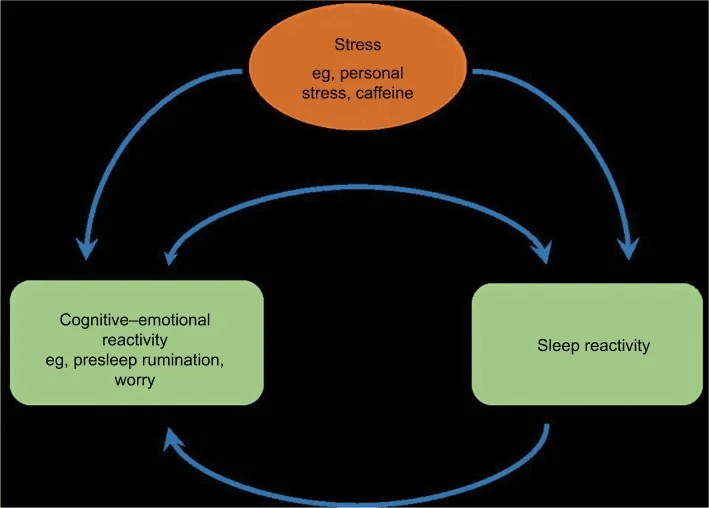
Possible feedback loop, between sleep reactivity and cognitive–emotional reactivity in response to stress
When to Pursue Clinical Evaluation For Sleep Breathing Evaluation
If your home observations or testing reveal consistent patterns of disrupted breathing, clinical evaluation becomes worthwhile. (Current guidelines recommend testing when apnea–hypopnea index (AHI) is ≥5 with symptoms or comorbidities, or ≥15 regardless of symptoms.)
Specifically, consider a sleep clinic if you:
- notice regular breathing pauses lasting 10+ seconds,
- oxygen saturation drops below 90%, or
- if home sleep testing shows an apnea-hypopnea index above 5 events per hour.
Persistent symptoms despite good sleep hygiene—chronic fatigue, morning headaches, difficulty concentrating—also warrant professional assessment, especially when combined with any breathing irregularities.
Don’t try to manage confirmed sleep-disordered breathing on your own. Untreated sleep apnea progressively affects cardiovascular health, cognitive function, and metabolic stability. Clinical sleep studies provide the detailed analysis needed for appropriate treatment selection—whether that’s CPAP therapy, oral appliances, positional devices, or surgical approaches.
The home data you’ve gathered becomes valuable context for your sleep specialist, helping them understand your specific patterns and tailor treatment accordingly.
4. So, You Have Ruled Out Sleep Apnea. What’s Left to Investigate?
Sleep Clinics Have Limited Tools for Non-Breathing Sleep Problems
You’ve ruled out sleep apnea—whether through formal testing, home assessment, or symptom patterns that don’t point toward airway instability.
But sleep quality remains poor.
This is a common experience. Sleep clinics excel at identifying breathing disorders, but when the issue isn’t airway-related, individuals often leave without clear next steps.
For many adults in midlife who wake up around 3 a.m. or feel unrefreshed despite adequate time in bed, the next place to look is how hormonal and autonomic systems work together to maintain sleep continuity.
1. The Neuro-Hormonal Influence on Sleep Stability (Testosterone / Estrogen / Progesterone Axis)
The stability of the second half of the night depends heavily on hormonal function. Testosterone, estrogen, and progesterone each act on the brain and shape the depth and continuity of sleep.
- Testosterone → NREM Integrity and Recovery
Healthy testosterone function supports deep, restorative sleep and overnight tissue repair. When this system requires greater support—as it often does with age or under chronic stress—deep-sleep continuity can weaken, leaving rest feeling lighter even when total hours are unchanged.
- Progesterone → GABA-A Support
Progesterone is a potent GABA-ergic agent, meaning it helps to calm the brain by acting on the same receptors as many sleep medications. It is critical for promoting and sustaining deep sleep (NREM). When progesterone function becomes less robust—during perimenopause, stress, or disrupted cycles—this natural brake on arousal is less effective, and awakenings become more likely.
- Estrogen → Thermoregulation and REM Continuity
Healthy estrogen function helps maintain serotonin synthesis and precise temperature control—both critical for REM stability. When estrogen function requires additional support, small fluctuations in core temperature can interrupt REM periods and trigger early-morning awakenings.
2. Autonomic Imbalance and the Body’s Stress-Regulation System (HPA Axis Reactivity)
Building on the neuro-hormonal role above, hormone function often needs more coordinated support with age to keep the HPA axis (the body’s stress-regulation network) steady through the night.
The body has a normal circadian rhythm where cortisol (your primary “wake” & “stress” hormone) is at its lowest around midnight and begins to gradually rise around 3 a.m. to prepare you for the morning.
Testosterone, estrogen, and progesterone interact with the HPA axis and can alter both stress reactivity and features of the 24-hour stress hormone rhythm.
- In a well-supported system: This gentle rise is imperceptible. You sleep through it.
- In a hormonally-sensitized system: When the functions of calming progesterone, stabilizing estrogen, and recovery-supporting testosterone require more support, the HPA (stress-response) axis becomes more reactive. The brain may misinterpret this normal, low-level cortisol rise as a stress signal causing you to wake up.
This triggers a shift to sympathetic (fight-or-flight) nervous system dominance.
The result is a awakening—often with a racing heart or active mind—that is difficult to reverse and fall back asleep, as your body is now biochemically in an “alert” state.
Sleep OS Hormones is now available as a 60-day self-guided program with dedicated systems for estrogen, progesterone, and testosterone, or bundled together for a more complete approach.
5. So, What Are Some Signs That Mid-Age Shift in Hormone Function Is Affecting Your Sleep?
Certain recurring patterns can point toward hormonal systems needing additional support to maintain sleep stability:
- Timing-specific awakenings: Waking around the same time each night (often 2–4 a.m.)
- Higher stress reactivity: Previously manageable stressors now disturb sleep
- Harder to fall back asleep: Brief awakening followed by prolonged alertness or mental activity
- Light, unrefreshing sleep: Adequate time in bed but unrested, sometimes with reduced deep-sleep percentages on wearables
- For men: A pattern of lighter, less restorative sleep combined with noticeable changes in daytime energy, recovery, or drive.
- For women (if still cycling): Noticeable sleep differences between luteal and follicular phases
- For women: Temperature sensitivity: Night sweats, feeling too warm, or heat intolerance that wasn’t present in earlier decades
These patterns aren’t exclusive to hormones, but when several appear together in midlife, hormonal support becomes one of the most impactful levers to restore sleep stability.
Even without lab confirmation, addressing these underlying systems—through structured support for testosterone, estrogen, and progesterone function—often produces meaningful improvement in both sleep quality and daytime resilience.
6. Rebuilding Sleep Stability Through Hormonal Support
The 3 a.m. pattern is often the outcome of shifts in the neuro-hormonal environment that accompany midlife.
These systems—testosterone, estrogen, progesterone, and their downstream effects on stress resilience and metabolic stability—typically require more support after age 40.
When that support is missing, fragmentation follows predictable patterns.
When it’s restored, sleep becomes steady again.
The goal is this: sleep that’s robust, not delicate—maintained by the body’s own internal regulation rather than external effort.
Warmly
—Kat
P.S. If your sleep has changed in midlife—lighter, shorter, or more reactive under stress—the underlying hormonal transitions are often the missing layer.
Sleep OS Hormones was built for this stage. It helps you support the testosterone–estrogen–progesterone pathways that underpin sleep stability and stress resilience.
You can see which Sleep OS Hormones framework fits your situation here:
Or, learn more about the most popular Trio Hormone Framework here
or the foundational Sleep–Stress Single Hormone Frameworks here


