Vitamin D For memory loss: Why Vitamin D Is a Brain Health Powerhouse—Not Just a Bone Supplement
Vitamin D for memory loss is gaining attention for good reason—this often-overlooked nutrient plays a far greater role in brain health than most people realize.
Forget what you thought you knew about vitamin D.
It’s not just about bone strength or calcium absorption. Vitamin D is a neuroactive compound—with wide-reaching benefits, including vitamin D for brain function, learning, and motivation.
Get Weekly Insights to Personalize Your Own Longevity Roadmap
Emerging research shows that vitamin D plays a powerful role in:
- Supporting neuroplasticity and neuronal growth
- Regulating mood, motivation, and mental energy
- Protecting the brain from inflammation, oxidative stress, and degeneration
In fact, low vitamin D levels are now being linked to faster cognitive decline and higher risk of neurodegenerative diseases like Alzheimer’s, Parkinson’s, and vascular dementia.

So if you’re supplementing casually… or assuming a little sun is enough… this article is for you.
Inside, we’ll cover:
- How vitamin D fuels cognitive performance and long-term brain health
- Why many people stay deficient—even when doing everything “right”
- A smarter, longevity-focused strategy for optimizing your vitamin D levels year-round
💡 This isn’t about avoiding rickets —it’s about vitamin D and brain health & cognitive performance for the long haul.
Table of Contents
🧠 Vitamin D and Cognitive Function: Neuroplasticity and BDNF
Vitamin D doesn’t just support the brain—it activates it.
At the cellular level, vitamin D helps regulate everything from neuroplasticity and neurogenesis to inflammation, calcium balance, and even neurotransmitter function. Its receptors (VDRs) are found throughout the brain—including in areas tied to memory, mood, and learning.
Here’s how it works, and why it matters if you care about staying sharp for the long haul:
A. Vitamin D and Neuroplasticity: How D3 Fuels Brain Adaptability
Vitamin D is a neuroactive compound that regulates how your brain forms new connections, adapts to stress, and protects itself from damage. At the center of this process is its influence on neuroplasticity—the brain’s ability to rewire and respond to learning, trauma, and experience.
Here’s what the science shows:
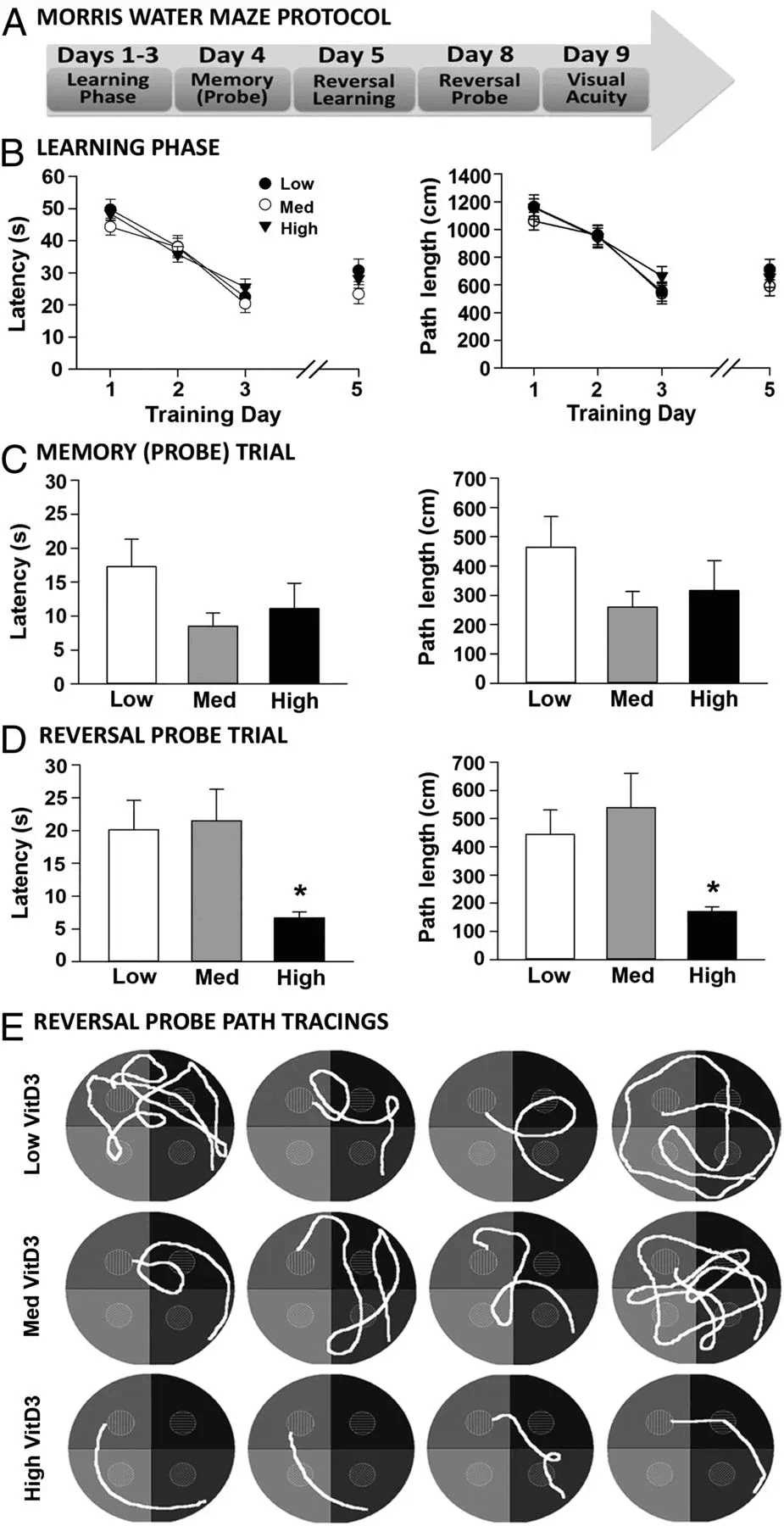
- BDNF & Synaptic Strengthening In mice, repeated administration of vitamin D3 (2.5 μg/kg over 21 days) led to a significant increase in BDNF (brain-derived neurotrophic factor) in the hippocampus and prefrontal cortex. These brain regions are key to memory and executive function. In the same study, vitamin D3 also boosted levels of TrkB (BDNF’s receptor), GluA1 (an AMPA receptor subunit), and synaptic scaffolding proteins like PSD-95 and synapsin—molecules essential for strong, resilient synaptic connections. This points to vitamin D3’s ability to drive structural synaptic plasticity, the literal building of new connections in the brain. These structural changes lay the groundwork for better vitamin D and cognitive function outcomes in both animal and human studies
- Protection Against Stress-Induced Neurodegeneration In a rat model of chronic stress, vitamin D3 supplementation reversed memory impairment and restored hippocampal BDNF levels. These animals also showed reduced oxidative stress and amyloid-beta accumulation—hallmarks of early neurodegenerative damage. The findings suggest that vitamin D doesn’t just enhance plasticity in ideal conditions—it actively protects it under metabolic and emotional stress. This highlights the potential of vitamin D for memory loss prevention by strengthening synaptic connections and hippocampal plasticity
- In Humans: Developmental Brain Impacts in Children Vitamin D deficiency in early pregnancy has been found to be associated with the disruption of fetal brain development and neurodevelopmental function (with impaired gross motor function.
Together, these findings suggest that vitamin D isn’t just “supportive” of brain health—it may be a molecular switch that turns on the machinery your brain needs to grow, adapt, and thrive.
B. Vitamin D and Brain Wiring: NGF, GDNF, and Dopaminergic Development
Vitamin D isn’t just supporting neuroplasticity—it’s shaping the wiring of the brain itself.
Beyond BDNF, this hormone-like vitamin activates other critical brain growth factors, including nerve growth factor (NGF) and glial cell-derived neurotrophic factor (GDNF). These molecules are essential for neuronal survival, especially in areas vulnerable to aging and degeneration.
Here’s what recent research reveals:
- NGF, GDNF, and Dopaminergic Survival
- Vitamin D directly boosts NGF, GDNF, and their receptors in neurons and glial cells—key players in synaptic health, emotional regulation, and executive function. In animal models, blocking vitamin D’s ability to increase GDNF removes its protective effects on dopamine neurons.
- This is a critical aging pathway: dopamine circuits are often the first to degrade in disorders like Parkinson’s.
- Neurite Growth and Synaptic Resilience
- Vitamin D stimulates neurite outgrowth—the structural extensions that allow neurons to connect and signal. In cultured neurons, adding 1,25(OH)₂D₃ (active vitamin D) sharply increased axonal growth, NGF release, and repair after injury or stress.
- It also restored growth in neurons with impaired epigenetic regulation—pointing to a genomic mechanism.
- Dopaminergic System Programming in Development
- In prenatal models, vitamin D deficiency disrupted the specification, placement, and maturation of dopamine-producing neurons in the midbrain—changes linked to long-term behavioral and cognitive issues.
- The effects mirror some of the same neural signatures seen in schizophrenia and ADHD.
But brain health isn’t just about growth and adaptation—it’s about protection, too. That’s where vitamin D steps in as one of the most underrated defenders of your neurons.
Vitamin D isn’t just supporting brain development—it’s directing it. It regulates gene expression in neurons, astrocytes, and microglia, promotes key growth factors like NGF and GDNF, and shapes dopamine circuits from early life into old age.
Vitamin D and Neuroprotection – How Vitamin D Reduces Inflammation, Oxidative Stress, and Calcium Overload
A brain that learns is essential. But a brain that lasts? That’s the longevity goal.
As we age, the challenges compound: chronic inflammation ramps up, oxidative stress weakens cellular defenses, and calcium balance begins to slip—leaving neurons overstimulated and vulnerable. These shifts don’t just correlate with aging—they help drive it.
Vitamin D is one of the few compounds with influence on all three of these core mechanisms.
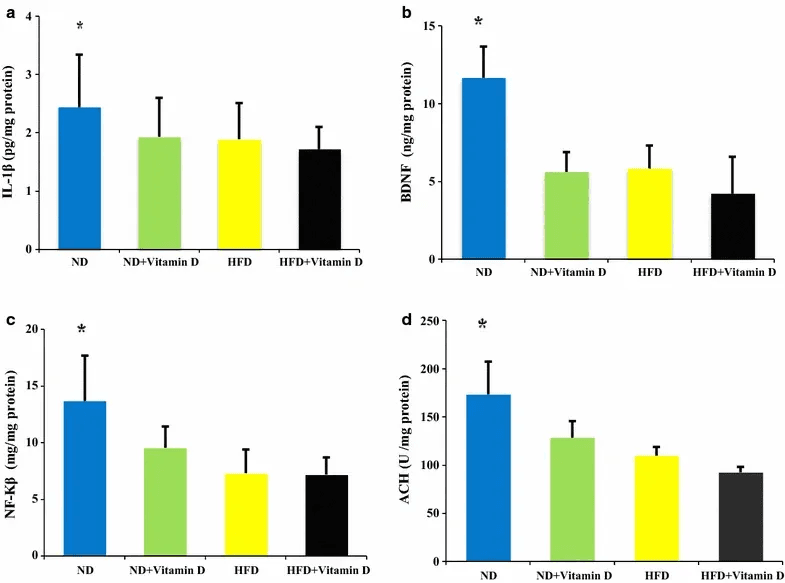
A. Vitamin D and Brain Inflammation: Lowering Cytokines That Harm Neurons
One hallmark of brain aging is an overactive inflammatory response. Elevated cytokines like IL-6 and TNF-α impair synaptic signaling, disrupt mood regulation, and are frequently observed in conditions like Alzheimer’s, Parkinson’s, and depression.
Vitamin D helps quiet this storm.
It interacts with immune cells in the brain and nudges them away from a pro-inflammatory state, acting as a modulator of neuroinflammation—particularly under metabolic stress or with age.
In one study, vitamin D supplementation reduced IL-1β and NF-κB in the hypothalamus of normal-diet rats and modulated some inflammatory markers in obese rats, supporting its potential as a neuroprotective agent in obesity-related cognitive decline.
B. Vitamin D and Oxidative Stress: Supporting the Brain’s Antioxidant Defense System
Every thought, every memory, every neuron firing comes at a cost: oxygen. Your brain runs hot—burning through 20% of the body’s oxygen—and that creates oxidative stress.
Normally, your cells manage this just fine. But as we age, that balance shifts. Antioxidant defenses decline, free radicals build up, and neurons begin to take damage they can’t repair. Left unchecked, this oxidative stress eats away at membrane integrity, mitochondrial function, and synaptic communication.
Vitamin D helps flip the balance back. It upregulates key antioxidant enzymes like superoxide dismutase (SOD) and catalase—molecules that neutralize reactive oxygen species before they damage neurons.
In animal studies, vitamin D3 reversed memory deficits caused by chronic stress and restored antioxidant enzyme activity in the hippocampus—the brain’s memory hub.
For longevity, this matters.
Oxidative stress is one of the earliest detectable drivers of neurodegeneration. It accelerates aging before symptoms appear. And vitamin D directly addresses it at the molecular level.
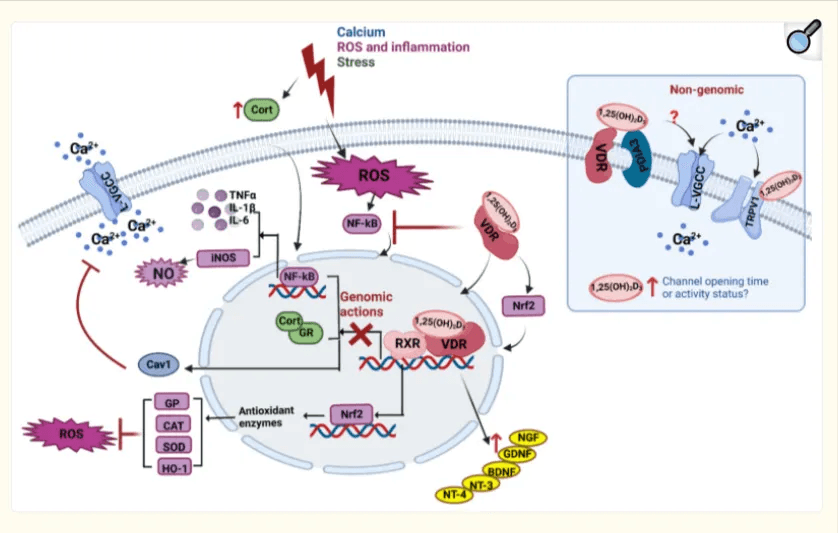
C. Vitamin D and Calcium Balance in the Brain: Preventing Excitotoxicity
Calcium is essential for brain function. It’s how neurons fire, how memories form, how thoughts take shape. But it’s also a double-edged sword.
Too much calcium inside a neuron is toxic. It triggers a process called excitotoxicity—a runaway loop of overstimulation that damages or kills brain cells. This kind of dysregulation is seen in both acute brain injuries and slow-burn neurodegenerative diseases.
Vitamin D helps prevent that overload.
It increases the expression of calcium-binding proteins and regulates calcium transport channels, keeping intracellular calcium in check. This tight control is critical for maintaining normal brain signaling—and ensures that brain signaling remains stable—an overlooked factor in vitamin D and cognitive function across aging.
For brain resilience over the decades, calcium balance is critical.
Why this matters for longevity:
Neurodegenerative diseases often take decades to develop. But the biochemical drivers—chronic inflammation, oxidative stress, and calcium dysregulation—start much earlier.
(By the way—vitamin B12 plays a different but equally important role in brain aging. If you’re interested in how low or borderline B12 can affect white matter, cognition, and methylation, you can read more about it here.)
D. Vitamin D and Memory Loss: Evidence Linking Deficiency to DementiaIf vitamin D protects neurons, calms inflammation, and boosts synaptic plasticity… what happens when you don’t have enough?
The answer isn’t speculative anymore.
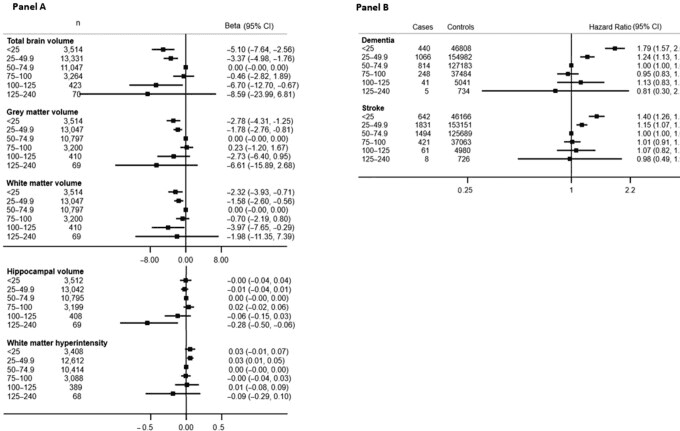
Large-scale studies suggest a significant role for vitamin D for memory loss, with lower levels linked to lower brain volume & significantly higher associations with Alzheimers & dementia:
- In a prospective study of 1,658 older adults free from dementia and cardiovascular disease at baseline, those with severe vitamin D deficiency (<25 nmol/L) had more than 2x the risk of developing dementia or Alzheimer’ compared to above 50 nmol/L (HR = 2.22).
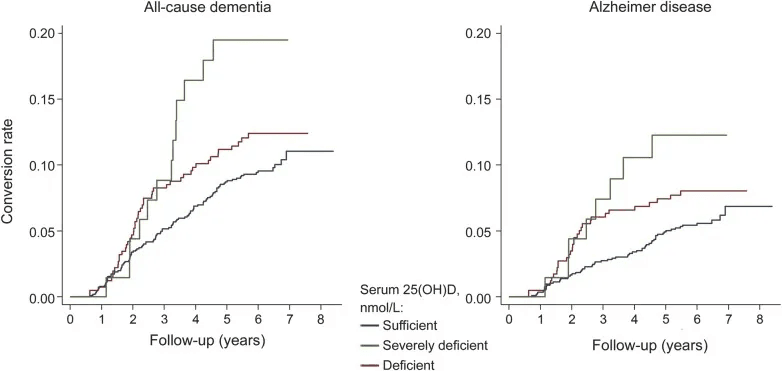
- A large-scale UK Biobank study following over 427,000 adults found that vitamin D deficiency (<25 nmol/L) was linked to a 79% higher risk of developing dementia, compared to those with levels in the 50–75 nmol/L range (adjusted HR: 1.79). Mendelian randomization analyses supported this as a potential causal relationship—not just a correlation—suggesting that increasing low vitamin D levels could prevent up to 17% of dementia cases.
- Brain imaging data linked lower vitamin D to reduced gray matter volume—especially in regions tied to memory and executive function. Data from a large population study shows the strongest risks in those with serum vitamin D levels below 25 nmol/L.
Animal research mirrors these patterns:
- Rodents with low vitamin D accumulate more amyloid-beta, display mitochondrial dysfunction, and show elevated markers of inflammation and calcium dysregulation—effects that parallel human neurodegenerative pathways. Supplementation in these models often reverses both the biological and behavioral damage. This supports the growing link between vitamin D and brain health, especially in aging populations
Longevity Takeaway:
Neurodegenerative diseases don’t appear overnight.
They build slowly—fueled by decades of low-grade inflammation, oxidative wear-and-tear, and disrupted calcium control.
Vitamin D is a nutrient that hits all three of those processes. And in both human and animal studies, lower levels consistently correlate with faster cognitive decline.
If you want a brain that lasts, don’t ignore your D status.
⚠️ A Word of Caution: When More Isn’t Better, Why Dosing Matters (The Inverted-U Problem)
If you’ve made it this far, you’ve probably had the same thought I did:
“If vitamin D is this powerful for brain health… why not just take more?”
It’s a fair instinct—but it backfires.
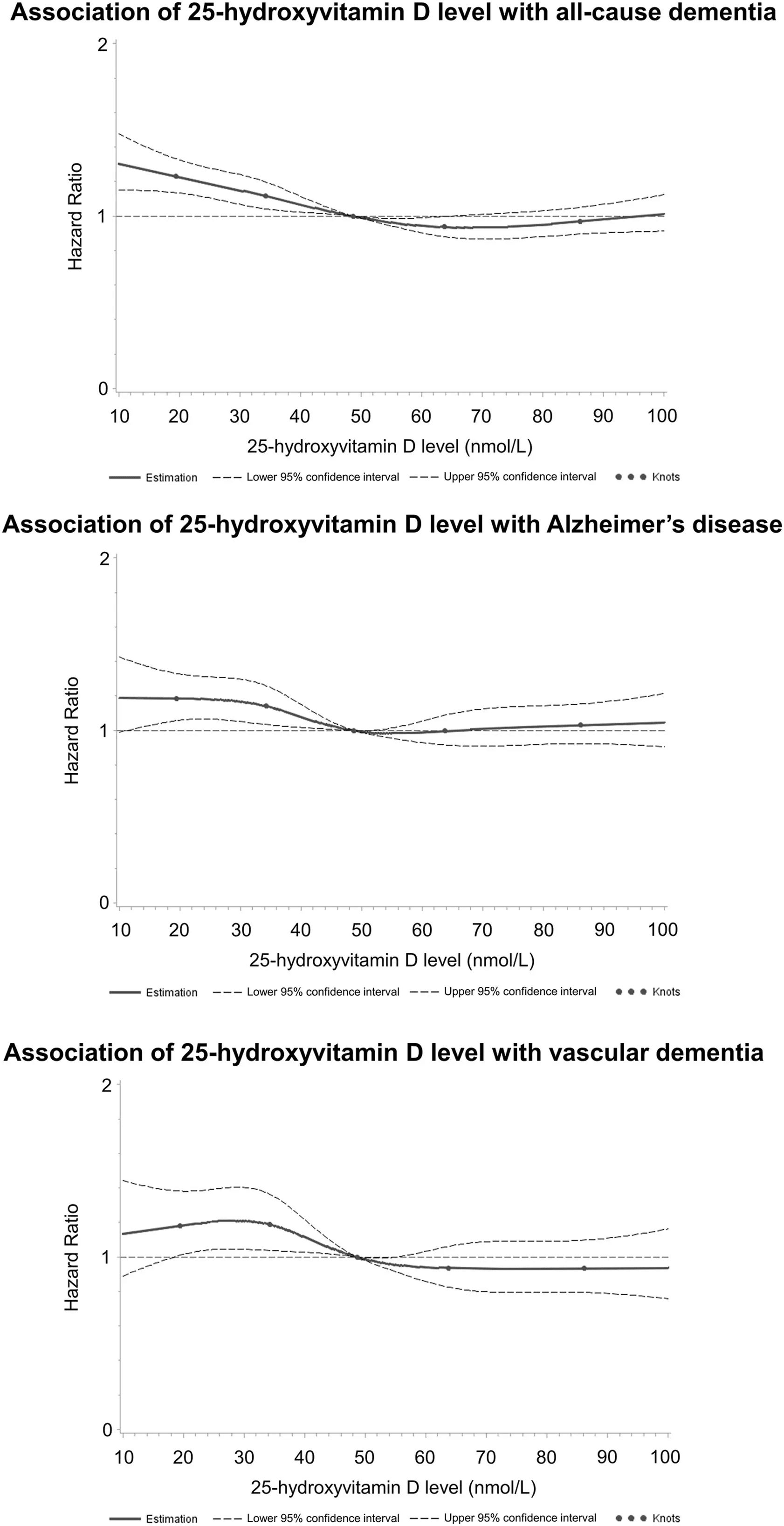
Vitamin D follows an inverted-U curve: too little and the brain suffers, but too much can impair signaling and increase neuronal stress. At higher levels, active vitamin D (1,25(OH)₂D₃) can disrupt calcium balance, alter brainwave activity, and—at extremes—accelerate neurodegeneration. Excess vitamin D intake can reduce brainwave activity due to calcium balance disruption. Mice with artificially high vitamin D levels aged faster and showed signs of blood-brain barrier breakdown and neuroinflammation.
And this isn’t just about mice.
In another 2024 UK biobank study with over 269,000 participants, shows the same U-shaped risk in humans. As illustrated in the chart below, both low and excessively high 25-hydroxyvitamin D levels were associated with worse dementia outcomes.
The lowest risk zone?
Right in the middle—around 60–75 nmol/L.
Even without going that far, unnecessarily high serum levels may do more harm than good.
This is why many longevity researchers now treat vitamin D not as a casual supplement, but as a neuroactive hormone.
It requires the right range, not maximum dosing.
So how do you get it right?
If high doses can backfire—and low levels put your brain at risk—then when it comes to vitamin D and brain health, precision is everything. But here’s the curveball: even when you’re doing the “right things,” your levels might still lag.
That’s where genetics, metabolism, and proper monitoring come in.
🧬Why You’re Still Vitamin D Deficient: Genetics, Metabolism, and Vitamin D Testing
You get outside when the sun’s out. You take your D3. Your diet isn’t a disaster.
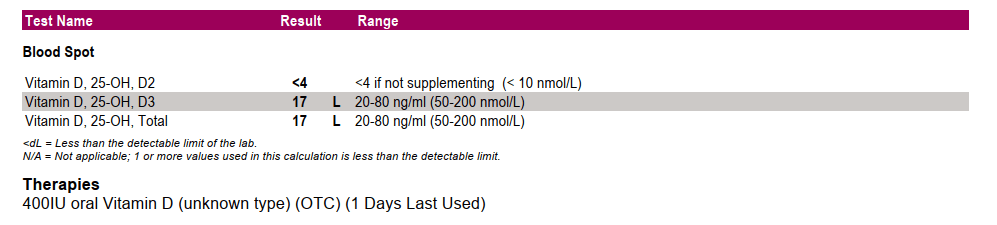
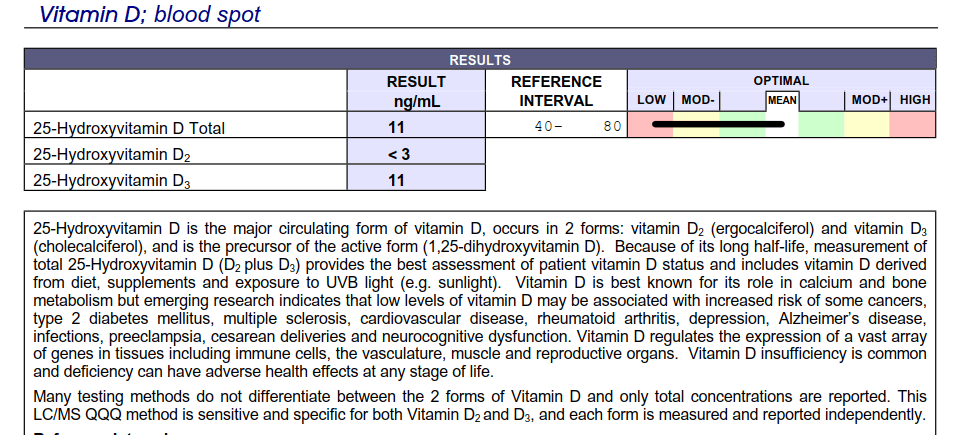
But then comes the vitamin D lab test—your levels are still low.
Frustrating? Yes.
Uncommon? Not at all.
For a surprising number of people, vitamin D deficiency isn’t about habits—it’s about genetics.
And if you’re not accounting for that, you may be stuck in a cycle of low energy, mood dips, and low-grade inflammation, all while thinking you’ve covered your bases.
Get Weekly Insights to Personalize Your Own Longevity Roadmap
When Sun and Supplements Aren’t Enough: Genetic Reasons for Vitamin D Deficiency – Why Some Bodies Don’t Respond
Vitamin D metabolism isn’t a straight line.
It’s more like a relay race involving multiple genes—each one playing a role in absorption, conversion, transport, activation, and degradation.
If even one of those genes misfires?
Your vitamin D status won’t behave as expected with sunshine & supplementation.
The Genetics of Vitamin D Metabolism: VDR, CYP2R1, and CYP24A1
Take CYP2R1—an enzyme in your liver that turns vitamin D into its main circulating form (25(OH)D). If you carry a variant of this gene, like rs10766197, you might convert less vitamin D, no matter how much sun you soak in or how high you dose.
Or DBP—the vitamin D–binding protein that moves D through the bloodstream. A variant called rs4588?
It’s been linked to an 11.5x higher chance of non-response to supplementation in otherwise healthy adults. Even CYP24A1, which normally breaks down excess vitamin D, can go into overdrive—degrading it too quickly and keeping your levels low despite consistent intake
How Common Are Genetic Vitamin D Deficiencies? Insights from Population Studies
Studies now show that these genetic differences explain a large portion of why vitamin D levels vary between individuals, even under similar lifestyle conditions.
- In one large study, people with multiple “risk alleles” had over double the risk of deficiency—even with standard supplementation.
- Another review identified multiple genes tied to low vitamin D status, including several that directly impact brain health pathways like calcium regulation and oxidative stress buffering.
This means your friend might hit 40 ng/mL on 1,000 IU/day… while you stay stuck at 20, even with 5,000 IU and midday sun.
The difference? Genetic metabolism.
Vitamin D Deficiency and Cognitive Decline: What You Need to Know
If you’ve been following the science so far, you know that low vitamin D affects neuroplasticity, inflammation, and calcium balance—three foundational pillars of cognitive aging.
But here’s the kicker: even mild deficiency has been linked to brain shrinkage on MRI, memory decline, and an > 50% increased risk of dementia over 11 years.
Now imagine if your body has been clearing vitamin D faster than you can replace it. That’s a deficiency you don’t want to sleep on.
Genetic variation influences how you absorb, convert, and retain vitamin D—which is why some people stay low, even when doing everything “right.”
If you’re not testing, you might never know.
By the way if that deficiency is paired with fragmented sleep? The brain takes a double hit.
This breakdown shows how poor REM sleep and sleep fragmentation accelerate structural brain decline—even in people with no symptoms.
5 Keys to Smart Vitamin D Optimization for Brain and Body
If vitamin D truly plays a protective role in brain aging, mood, immune regulation, and neuroplasticity — then getting your levels right isn’t just a wellness trend.
It’s a practical, long-game move.
But here’s what many people get wrong, including some health care providers:
Optimization doesn’t start with high-dose supplementation.

It starts with understanding how your body makes, absorbs, and manages vitamin D — and how those pathways vary based on your skin tone, location, genetics, and lifestyle.
Here’s what matters, and how to approach it with intention:
A. Sunlight and Vitamin D: Why Skin Synthesis Isn’t Always Enough
Most of your vitamin D is synthesized when UVB rays hit your skin and trigger the conversion of 7-dehydrocholesterol to pre-vitamin D3. In theory, this means we should get plenty of it by simply spending time outdoors.
In practice, it’s more complicated.
The efficiency of this process drops dramatically depending on:
- Skin tone: Higher melanin content reduces UVB absorption. People with darker skin may need significantly more sun exposure to generate the same amount of vitamin D. Individuals with darker skin (e.g., Fitzpatrick skin types IV–VI) require 3–6 times more UVB exposure than those with lighter skin (types I–II) to produce equivalent vitamin D levels. For example, a light-skinned person might need 10–15 minutes of midday sun, while a dark-skinned person might need 30–60 minutes or more, depending on UVB intensity.
- Geography and season: Above 37° latitude — think New York, Oslo, or Tokyo — winter sunlight isn’t strong enough to trigger much D synthesis, no matter how long you’re outside.
- Time of day: Midday sun (10 a.m. to 2 p.m.) delivers the highest UVB levels. Morning and evening light, even if pleasant, doesn’t do the job. Exposure during midday can produce 2–3 times more vitamin D than early morning or late afternoon exposure of the same duration
- Age: Older adults have less 7-dehydrocholesterol in the skin, making synthesis less efficient. With age, we need more sun exposure or supplementation to achieve adequate levels
- Sunscreen and clothing: Even SPF 15 can reduce vitamin D production by over 90%. Clothing can also prevent UVB penetration, with coverage (e.g., long sleeves, hats) effectively eliminating synthesis in covered areas
This variability is why even people who get outdoors regularly often test low — especially in late winter and early spring. It’s also why sun exposure alone isn’t a reliable strategy for most people living outside the tropics.
B. Vitamin D in Food: Helpful, But Not Sufficient
Vitamin D is one of the few nutrients not easily obtained from food — and modern diets don’t do much to help.
Still, some whole food sources contribute meaningfully:
- Fatty fish: A 100-gram serving of wild salmon can deliver 400–600 IU of vitamin D3. Mackerel and sardines also contain 150–600 IU of vitamin D3 per 100 grams.
- Egg yolks: One large yolk provides about 40 IU.
- UV-exposed mushrooms: These contain D2 (ergocalciferol), which is less bioavailable but still contributes. Levels vary widely: wild chanterelles have ~100–200 IU/100g, while UVB-treated maitake or portobello can reach 400–1,000 IU/100g. Its worth noting that D2 is less effective at raising serum 25(OH)D levels than D3 (by ~30–50%).
- Fortified foods: Some milks, cereals, and plant-based alternatives are fortified with D2 or D3, typically around 100 IU per serving.
Even with a well-rounded diet, total daily intake often hovers under 300 IU — below what’s considered optimal for vitamin D for brain health and immune health.

Optimal Levels: The Recommended Dietary Allowance (RDA) from the Institute of Medicine is 600 IU/day for adults (up to 70) and 800 IU/day for those over 70. However, many experts argue for higher intakes (1,000–4,000 IU/day) for optimal brain and immune function
C. Vitamin D Blood Tests: What to Check and When to Test
Vitamin D status is assessed via blood levels of 25-hydroxyvitamin D (25(OH)D), not through symptoms alone. Two people with similar diets and sun habits can show drastically different levels — which is why regular testing is non-negotiable if you want to optimize.
- How to test for Vitamin D: Ask for a 25(OH)D vitamin D blood test. Getting a vitamin D lab test is easier than ever -Most labs now offer both in-clinic and an at-home vitamin D test.
- When to test: At minimum, twice per year — end of winter (lowest point) and end of summer (highest point).
- Optimal range:
- ng/mL: Maintaining 40–60 ng/mL may support immune resilience, mood regulation, and vitamin D for brain function.
- nmol/L: Equivalent to 100–150 nmol/L.
- Deficiency thresholds:
- Below 20 ng/mL (50 nmol/L) is considered deficient.
- Below 10 ng/mL (25 nmol/L) is associated with more serious health risks, including bone loss and cognitive decline.
If your levels are within range, hold the course. If not, it’s time to adjust.
D. How to Supplement Vitamin D Safely and Effectively
For many people — especially those living in northern latitudes or with darker skin — supplementation becomes necessary. But it needs to be individualized.
- Common safe range:
- 1,000 to 2,000 IU per day is safe and sufficient for most adults.
- 4,000 IU per day is generally considered the upper safe limit.
- Forms:
- Choose vitamin D3 (cholecalciferol) for better absorption over D2.
- Take with fat:
- Because it’s fat-soluble, vitamin D should ideally be taken with a meal that contains some dietary fat.
And remember: more isn’t better.
Overshooting into the high 80s or 90s ng/mL doesn’t offer added protection — and may actually be harmful, especially to the brain. We covered this in Section 2 under hypervitaminosis D.
E. Best Times to Get a Vitamin D Lab Test
If you do nothing else — test in March (end of winter) and again in September (end of summer) – if you are in the northern hemisphere. You’ll know where you stand at both your lowest and highest points, and whether your current habits are working.
Most people find their winter numbers tell the real story. That’s where optimization matters most.
How to Personalize Your Vitamin D for Brain Health & Longevity
Because of genetic variability, there’s no “standard dose” of vitamin D intake that works for everyone. Without blood testing, you’re just guessing. And timing matters too.
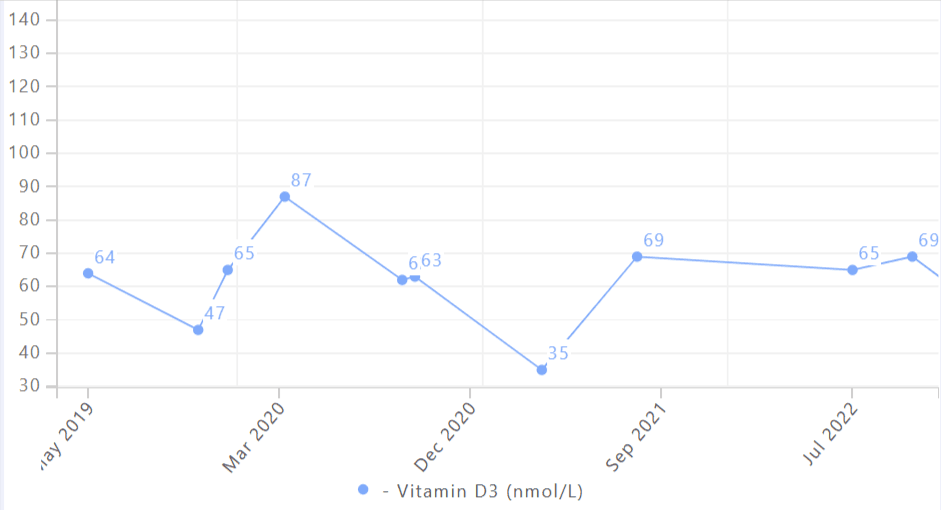
For most people in the northern hemisphere, March marks the low point—after a long, low-sun winter. If you only run a vitamin D test once a year, make it then. If you’re in the southern hemisphere, shift that window to September, following your own winter season.
Wondering why you feel foggy or flat around late winter? This might be why.
Vitamin D isn’t just a nutrient. It’s a neuroactive steroid hormone—with long-tail consequences when out of balance. And for longevity?
Consistent balance is everything.
Once you’ve tested and established your baseline, the real work begins—not with guesswork or megadosing, but with steady, informed decisions that align with your body’s needs.
Get Weekly Insights to Personalize Your Own Longevity Roadmap
Here’s how we think about implementation inside The Longevity Vault:
A. Run a Vitamin D Panel 2x a Year—Or More If You Want Precision
As we’ve discussed earlier, the most practical place to start is with two Vitamin D blood tests per year. An at home vitamin D test can help you track seasonal drops without needing a clinic appointment. Once in late winter (March) when your levels are lowest, and once at the end of summer (September) when sun exposure is highest.
These two points give you a natural high-low range to work from.
Why an At Home Vitamin D Test Might Be Best
If you’re aiming to fine-tune your protocol—for example, adjusting based on how your levels respond to a specific supplement dose or sun exposure routine—test more often. Every 3–4 months is reasonable during optimization phases and an at home vitamin D test might be most suited.
Why?
Because published dosing guidelines (like 1,000 IU = 10 ng/mL increase) don’t hold up well across individuals. Genetics, absorption, skin tone, and baseline levels all impact how much your serum vitamin D moves per IU. Testing is the only way to see what your body actually does.
B. If You Want Finer Control, Test Your Genes—But Don’t Stop There
Genetic testing can provide insight into how your body processes vitamin D—especially genes like:
- VDR (Vitamin D Receptor): Impacts how cells respond to vitamin D.
- CYP2R1: Affects conversion of D3 to 25(OH)D.
- GC (Vitamin D Binding Protein): Regulates how vitamin D is transported in the blood.
These variations can help explain why some people remain low despite normal intake. But genetic data alone can’t tell you how much you personally need to reach optimal levels. It’s useful context—but blood levels still determine dosing.
C. Avoid High-Dose Vitamin D Supplementation Without Data
Some GPs still prescribe vitamin D supplements at 50,000 IU weekly—a practice that may be appropriate in cases of severe deficiency, but often isn’t personalized.
These doses can spike levels too high, too fast—especially if taken without retesting. In some people, they may lead to side effects like fatigue, headaches, or calcium imbalance.
Unless you’re working with a clinician who’s testing and adjusting frequently, daily or every-other-day dosing at lower amounts is typically safer and more physiologic. This approach mirrors the body’s natural rhythm and avoids the peaks and crashes seen with large boluses.
D. Use Vitamin D Test Kits to Track Levels Over Time—Not Just a Snapshot
Like any longevity biomarker, vitamin D status is dynamic. It changes with season, travel, illness, and even body weight shifts. The best way to make sense of this is to track your levels over time—ideally using a combination of vitamin D test kits and a simple log like a journal, spreadsheet, or app. Testing every few months gives you a low-effort way to spot trends and fine-tune your protocol as needed.
Make note of:
- Date and results of vitamin D blood tests
- Supplement dose and brand
- Time spent outdoors (weekly average)
- Changes in diet (e.g. more oily fish, less dairy)
- Energy, mood, or cognitive changes (subjective, but useful)
Patterns emerge fast when you track—and that’s when real personalization begins.
E. Adjust Intake Seasonally—Not Just Annually
If you live at higher latitudes, your vitamin D synthesis from sun exposure drops to near zero during winter. That means your needs aren’t static.
- In summer: You may need little or no supplementation if you’re getting good sun exposure.
- In winter: You may need full-dose support to maintain levels. This could range from 1,000 to 4,000 IU/day, depending on your vitamin D test results and lifestyle.
Think of this like adjusting clothing to the season. You don’t wear a parka in July—or skip it in January. Your supplementation should follow the same logic.
F. Why Take Vitamin D3 with K2 for Brain and Bone Health
Vitamin D works upstream. It helps you absorb calcium. But without enough vitamin K2, that calcium doesn’t always end up in the right place.
That’s why it can be beneficial to take a vitamin D3 with K2 for optimal absorption and for the role of vitamin D and brain health.
It’s a subtle interaction, but over years, it matters. Many high-quality supplements now combine cholecalciferol (vitamin D3) with K2, making this step easy.
Just make sure the K2 form and dose are clearly listed—MK-7 has a longer half-life and is typically preferred for once-daily dosing.
📫 Your Next Step: Test Your Vitamin D Levels. Protect Your Brain.
Let’s make this practical.
Start by asking yourself:
When was the last time you checked your vitamin D levels?
Do you know how much they fluctuate across seasons?
Do you know how much vitamin D you actually need to stay in the optimal range year-round?
If the answer is “not really”—you’re not alone. But this is the kind of clarity that changes your long-term trajectory.
Let’s fix that:
› 1. Run a Vitamin D test.
If it’s been over a year—or you’ve never tested—it’s time. You can’t optimize what you can’t measure.
📞 Call your GP and request a vitamin D blood test (specifically a 25(OH)D test). Important: ask for the number, not just “you’re fine”.
› 2. Prefer to skip the clinic?
Or want a Vitamin D3 lab test more frequently than your GP will give you? We’ve made it simple.
💡 Shipped directly to your door. No appointment needed.
› 3. Review your results and adjust.
Whether you use an at home vitamin D test or an in clinic vitamin D lab test, the result gives you a measurable way to improve. if your level’s under 40 ng/mL, you might need to bump your dose, tweak your sun exposure, or add something like K2.
Most people respond to 1,000–2,000 IU/day, but it depends on your baseline, and how fast your levels rise given.
› 4. Re-run your vitamin D test and fine-tune.
Check again in 8–12 weeks to see how your levels respond. Adjust up or down based on that.
› 5. Still low despite doing “everything right”?
🧬 It could be genetic. Some people carry variants that affect absorption, transport, or conversion.
Some GPs prescribe high-dose vitamin D—like 50,000 IU doses. But that doesn’t mean it’s automatically the right move for you. Before going that route, it might be worth checking your genes. You can explore the DNA test I’ve used myself to get a clearer picture.
That said, the quickest insight often comes from a blood spot test.
FAQ – Vitamin D and Brain Health
Is vitamin D good for memory?
Yes—research increasingly supports the role of vitamin D for memory loss prevention and cognitive performance. Vitamin D supports BDNF (a growth factor tied to memory formation) and protects the hippocampus, your brain’s memory hub, from inflammation and oxidative stress. Low levels are consistently linked to faster memory decline and higher dementia risk. Optimizing your levels with the help of an at home vitamin D test is one of the most actionable steps you can take to protect long-term brain health.
That said, vitamin D isn’t the only nutrient with this profile. Low B12—especially when active forms are missing—has also been linked to subtle memory decline, even when blood levels appear normal.
How much does a vitamin D test cost?
The cost of a vitamin D test varies depending on where and how you take it. In clinics, a vitamin D blood test ordered through your GP can range from $50 to $150, especially if it’s not covered by insurance.
For convenience and privacy, many people now use at home vitamin D test kits, which typically cost between $50 and $90. These tests are easy to use, require just a small finger prick, and provide results in a few days—making them a practical option if you want to monitor levels more regularly or without a doctor’s visit.
💡 Inside the Longevity Essentials Labshop, we offer vetted vitamin D lab test kits that ship directly to your door.
What are signs of low vitamin D?
Low vitamin D can present in subtle but wide-ranging ways. Common signs include fatigue, low mood, frequent illness, muscle weakness, and trouble concentrating. From a brain health perspective, signs of low vitamin D may include forgetfulness, slower mental processing, or trouble focusing—especially during darker months. If you’re noticing these, it may be time to consider a vitamin D test or vitamin D lab test to check your baseline. Hair thinning and increased shedding are also common but overlooked signs of vitamin D deficiency, which I explore in detail in The Overlooked Link Between Vitamin D and Hair Loss.
What kind of vitamin D test should I get?
The most common vitamin D test is the 25(OH)D blood test, available both in clinics and through home kits. It’s the best way to track your actual levels and guide your next steps
Does a vitamin D blood test require fasting?
No, a vitamin D blood test doesn’t require fasting. You can take it at any time of day.
How much Vitamin D do I need for brain health?
Most research suggests that for vitamin D for brain health and mood regulation, the optimal vitamin D level is 40–60 ng/mL (or 100–150 nmol/L). This range appears to support neuroplasticity, inflammation regulation, and dopaminergic function—all critical if you’re concerned about vitamin D for memory loss or early cognitive decline.
While the current RDA for adults is just 600–800 IU, that’s based on bone health—not neurological protection. For brain benefits, most longevity-focused protocols recommend daily intakes between 1,000 and 2,000 IU, though this depends on your baseline level, skin tone, and sun exposure. The only way to know what you need is to test.
Can I get too much Vitamin D?

Yes. Vitamin D follows an inverted-U curve, where too little or too much can impair health. Hypervitaminosis D—usually caused by high-dose supplementation over time—can lead to hypercalcemia, which affects brain function, mood, and even neural conductivity.
Some physicians still prescribe vitamin D supplements at 50,000 IU, typically weekly, for short-term repletion. But outside of deficiency correction under medical supervision, this is not recommended for ongoing use. Most people do well within the 1,000–4,000 IU daily range. If you’re supplementing aggressively, blood testing is essential.
Why do my levels stay low despite supplements?
Several factors can blunt your response to supplementation:
Genetic variants (in VDR, DBP, CYP2R1) can reduce how well your body converts or transports vitamin D.
Obesity sequesters vitamin D in fat tissue.
Magnesium deficiency may impair vitamin D metabolism.
Poor absorption, especially with gut issues or when taken without dietary fat.
This is why we emphasize testing—not guessing. You may need higher doses, better timing, or cofactor support, but you won’t know without a vitamin D lab test to confirm your baseline and guide your protocol.
Is D2 or D3 better?
D3 (cholecalciferol) is the clear winner. It raises blood levels more effectively and stays active in the body longer than D2 (ergocalciferol). D3 is also the form your skin makes from sunlight.
Most high-quality supplements use D3. D2 is typically found in prescriptions and fortified foods but is less bioavailable for most people.
Conclusion: Turn Vitamin D Knowledge Into a Brain Health Protocol
By now, you’ve seen what vitamin D does for the brain—and how much individual variability affects whether you’re actually getting enough.
If cognitive clarity and protecting against memory loss are priorities, vitamin D needs a closer look.
Deficiency can linger even with good habits. And both low and high levels carry risks.
So the real question is:
Do you know where your levels stand right now?
If not, that’s the next move. Testing gives you a baseline. From there, it’s about adjusting, retesting, and—if needed—checking for deeper factors like genetic variation.
You don’t need to overhaul your life. You just need a process. If you’re not sure where to start, jump to this section for a step-by-step guide.
That’s it. That one data point—your vitamin D level—could be the most practical & actionable lever for optimizing vitamin D and cognitive function over decades.
If you’re ready to go a step further, we’ve also curated a shortlist of foundational tests—basic labs that cover common longevity blind spots. These can help round out your strategy beyond vitamin D. You can explore those here.
And if you want to see what this process looks like in real life—how I went from winter deficiency to stable levels—read my full vitamin D protocol here.
→ My Vitamin D Protocol: How I Solved My Winter Deficiency After 4 Years of Tracking
References
- Menéndez SG, Manucha W. Vitamin D as a Modulator of Neuroinflammation: Implications for Brain Health. Curr Pharm Des. 2024;30(5):323-332. doi: 10.2174/0113816128281314231219113942. PMID: 38303529.
- Chen LJ, Sha S, Stocker H, Brenner H, Schöttker B. The associations of serum vitamin D status and vitamin D supplements use with all-cause dementia, Alzheimer’s disease, and vascular dementia: a UK Biobank based prospective cohort study. Am J Clin Nutr. 2024 Apr;119(4):1052-1064. doi: 10.1016/j.ajcnut.2024.01.020. Epub 2024 Jan 29. PMID: 38296029; PMCID: PMC11007746.
- Philippou E, Hirsch MA, Heyn PC, van Wegen EEH, Darwish H. Vitamin D and Brain Health in Alzheimer and Parkinson Disease. Arch Phys Med Rehabil. 2024 Apr;105(4):809-812. doi: 10.1016/j.apmr.2023.10.023. Epub 2024 Jan 6. PMID: 38189701.
- Littlejohns TJ, Henley WE, Lang IA, Annweiler C, Beauchet O, Chaves PH, Fried L, Kestenbaum BR, Kuller LH, Langa KM, Lopez OL, Kos K, Soni M, Llewellyn DJ. Vitamin D and the risk of dementia and Alzheimer disease. Neurology. 2014 Sep 2;83(10):920-8. doi: 10.1212/WNL.0000000000000755. Epub 2014 Aug 6. PMID: 25098535; PMCID: PMC4153851.
- Navale SS, Mulugeta A, Zhou A, Llewellyn DJ, Hyppönen E. Vitamin D and brain health: an observational and Mendelian randomization study. Am J Clin Nutr. 2022 Aug 4;116(2):531-540. doi: 10.1093/ajcn/nqac107. PMID: 35451454; PMCID: PMC9348994.
- Shi Y, Shi Y, Jie R, He J, Luo Z, Li J. Vitamin D: The crucial neuroprotective factor for nerve cells. Neuroscience. 2024 Nov 12;560:272-285. doi: 10.1016/j.neuroscience.2024.09.042. Epub 2024 Sep 27. PMID: 39343160.
- Menéndez SG, Manucha W. Vitamin D as a Modulator of Neuroinflammation: Implications for Brain Health. Curr Pharm Des. 2024;30(5):323-332. doi: 10.2174/0113816128281314231219113942. PMID: 38303529.
- C.S. Latimer, L.D. Brewer, J.L. Searcy, K. Chen, J. Popović, S.D. Kraner, O. Thibault, E.M. Blalock, P.W. Landfield, & N.M. Porter, Vitamin D prevents cognitive decline and enhances hippocampal synaptic function in aging rats, Proc. Natl. Acad. Sci. U.S.A. 111 (41) E4359-E4366, https://doi.org/10.1073/pnas.1404477111 (2014).
- Kuźma E, Soni M, Littlejohns TJ, Ranson JM, van Schoor NM, Deeg DJ, Comijs H, Chaves PH, Kestenbaum BR, Kuller LH, Lopez OL, Becker JT, Langa KM, Henley WE, Lang IA, Ukoumunne OC, Llewellyn DJ. Vitamin D and Memory Decline: Two Population-Based Prospective Studies. J Alzheimers Dis. 2016;50(4):1099-108. doi: 10.3233/JAD-150811. PMID: 26836174; PMCID: PMC5525144.
- Cui X, Eyles DW. Vitamin D and the Central Nervous System: Causative and Preventative Mechanisms in Brain Disorders. Nutrients. 2022 Oct 17;14(20):4353. doi: 10.3390/nu14204353. PMID: 36297037; PMCID: PMC9610817.
- Häusler D, Torke S, Peelen E, Bertsch T, Djukic M, Nau R, Larochelle C, Zamvil SS, Brück W, Weber MS. High dose vitamin D exacerbates central nervous system autoimmunity by raising T-cell excitatory calcium. Brain. 2019 Sep 1;142(9):2737-2755. doi: 10.1093/brain/awz190. Erratum in: Brain. 2019 Nov 1;142(11):e64. doi: 10.1093/brain/awz249. PMID: 31302671; PMCID: PMC6736324.
- Farhangi, M.A., Mesgari-Abbasi, M., Nameni, G. et al. The effects of vitamin D administration on brain inflammatory markers in high fat diet induced obese rats. BMC Neurosci 18, 81 (2017). https://doi.org/10.1186/s12868-017-0400-1
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.
- Dhamayanti M, Noviandhari A, Supriadi S, Judistiani RT, Setiabudiawan B. Association of maternal vitamin D deficiency and infants’ neurodevelopmental status: A cohort study on vitamin D and its impact during pregnancy and childhood in Indonesia. J Paediatr Child Health. 2020 Jan;56(1):16-21. doi: 10.1111/jpc.14481. Epub 2019 May 6. PMID: 31062441.
- Kouba BR, Torrá ACNC, Camargo A, Rodrigues ALS. The antidepressant-like effect elicited by vitamin D3 is associated with BDNF/TrkB-related synaptic protein synthesis. Metab Brain Dis. 2023 Feb;38(2):601-611. doi: 10.1007/s11011-022-01115-0. Epub 2022 Nov 9. PMID: 36350480.
- Rozmus D, Płomiński J, Augustyn K, Cieślińska A. rs7041 and rs4588 Polymorphisms in Vitamin D Binding Protein Gene (VDBP) and the Risk of Diseases. Int J Mol Sci. 2022 Jan 15;23(2):933. doi: 10.3390/ijms23020933. PMID: 35055118; PMCID: PMC8779119.
- J.B. Cheng, M.A. Levine, N.H. Bell, D.J. Mangelsdorf, & D.W. Russell, Genetic evidence that the human CYP2R1 enzyme is a key vitamin D 25-hydroxylase, Proc. Natl. Acad. Sci. U.S.A. 101 (20) 7711-7715, https://doi.org/10.1073/pnas.0402490101 (2004)
- Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol. 2014 Mar 20;21(3):319-29. doi: 10.1016/j.chembiol.2013.12.016. Epub 2014 Feb 13. PMID: 24529992; PMCID: PMC3968073.
- Beydoun MA, Beydoun HA, Li Z, Hu YH, Noren Hooten N, Ding J, Hossain S, Maino Vieytes CA, Launer LJ, Evans MK, Zonderman AB. Alzheimer’s Disease polygenic risk, the plasma proteome, and dementia incidence among UK older adults. Geroscience. 2024 Nov 26. doi: 10.1007/s11357-024-01413-8. Epub ahead of print. PMID: 39586964.
- Korewo-Labelle D, Karnia MJ, Myślińska D, Kaczor JJ. Supplementation with Vitamin D3 Protects against Mitochondrial Dysfunction and Loss of BDNF-Mediated Akt Activity in the Hippocampus during Long-Term Dexamethasone Treatment in Rats. Int J Mol Sci. 2023 Sep 11;24(18):13941. doi: 10.3390/ijms241813941. PMID: 37762245; PMCID: PMC10530487.