In our previous article, we explored how interleukin-6 (IL-6) acts as an early warning signal—one that links low-grade inflammation to accelerated aging, cognitive decline, and long-term disease risk.
But understanding IL-6 is just the beginning.
The real question is: how can you use and interleukin 6 test (IL-6 test) to make smarter, earlier decisions about your healthspan and longevity strategy?
Get Weekly Insights to Personalize Your Own Longevity Roadmap
Most doctors only check IL-6 when you’re already seriously ill—like during sepsis or autoimmune flares. But for longevity optimization, we approach it differently.
Longevity isn’t about reacting after damage shows up.
It’s about knowing your baselines—and acting before the shift becomes difficult to reverse.
IL-6 can detect inflammation years before symptoms appear—offering a chance to protect brain health, metabolism, and long-term resilience.
Unlike CRP, which only tells you that inflammation exists, IL-6 can help you understand where it’s coming from and how active it is. And that’s what makes it a powerful tool for optimization & prevention, not just disease care.
In this article, we’ll break down when IL-6 testing matters most, how to interpret results in context, and how those results can refine your next steps—especially if you’re already focused on prevention.
Table of Contents
1. Who Might Want To Consider An Interleukin 6 Test (IL-6 Test) for Inflammation and Longevity
An interleukin 6 lab test isn’t just for patients with known disease.
It’s a proactive tool for identifying early, subclinical inflammation—especially in cases where traditional labs like CRP appear normal or only mildly elevated—and for refining risk stratification before disease becomes clinically obvious.
Whether your CRP is elevated, borderline, or normal, measuring IL-6 can reveal inflammatory processes that may otherwise go unnoticed—helping you make more targeted decisions sooner.
Here’s when you might want to consider ordering an interleukin 6 lab test:
Persistent Mildly Elevated CRP, But You’re Still Stuck
You’ve cleaned up your diet. You’ve lost weight. You’ve added regular workouts.
And yet… your CRP or hs-CRP won’t budge—still floating in the 1.5–5 mg/L range.
This is where IL-6 can tell you what CRP can’t.
CRP elevated + IL-6 elevated:
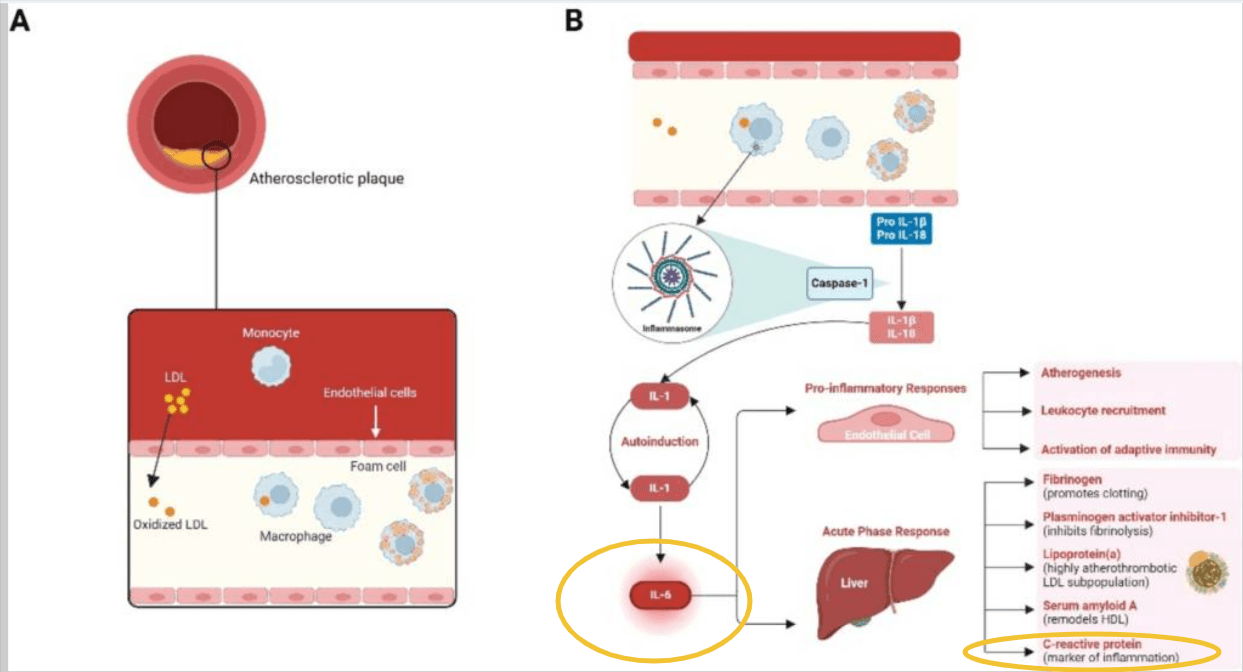
If both CRP and IL-6 are elevated, that’s a sign of ongoing active inflammation—driven by tissue-specific stressors:
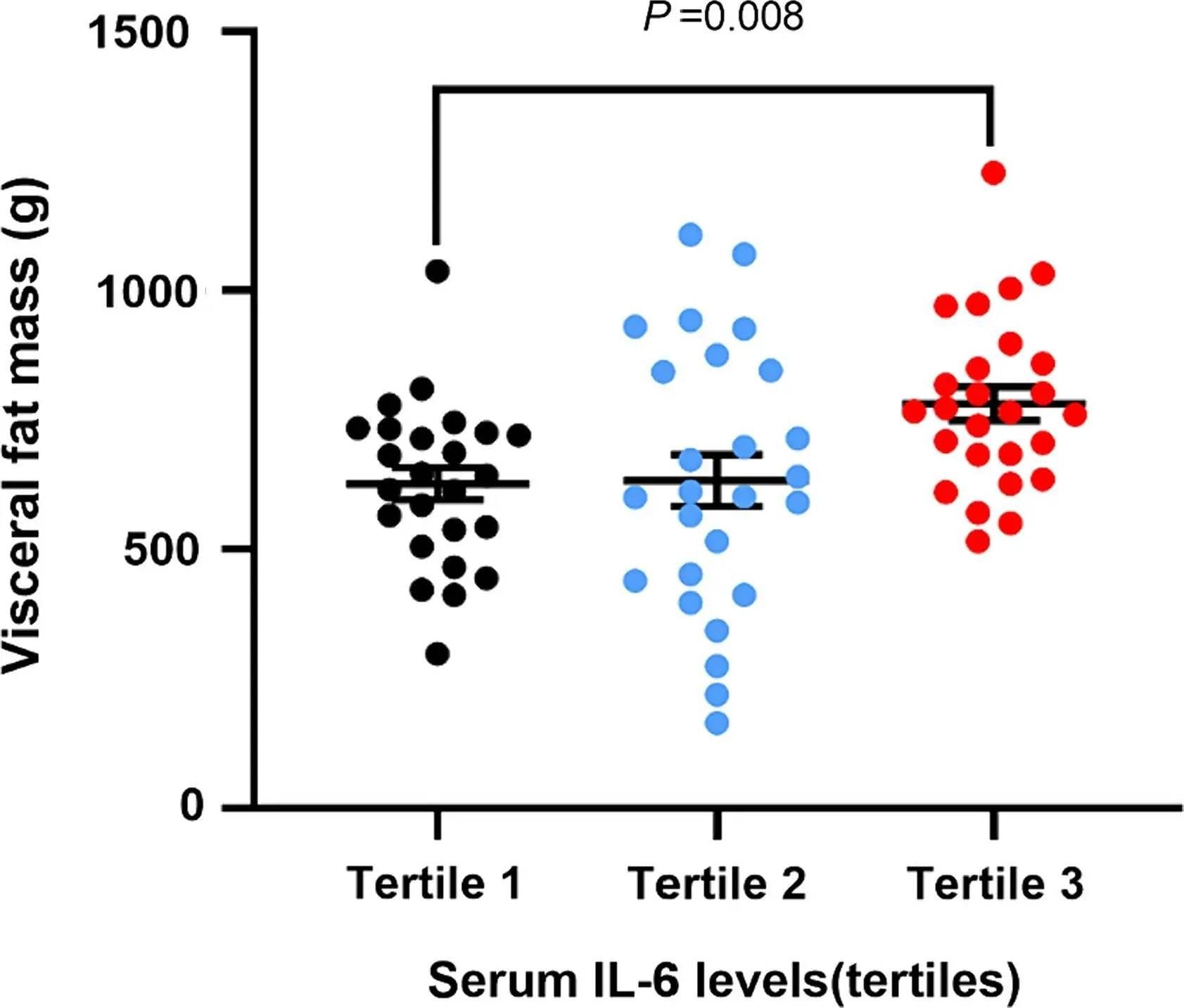
- Visceral fat can keep immune signaling high, even at a healthy weight.
- Post-exercise muscle inflammation can cause short-term spikes.
- Neural inflammation may be contributing without obvious symptoms.
- Or, there could be early autoimmune activation—which won’t show up on ANA or RF until much later.
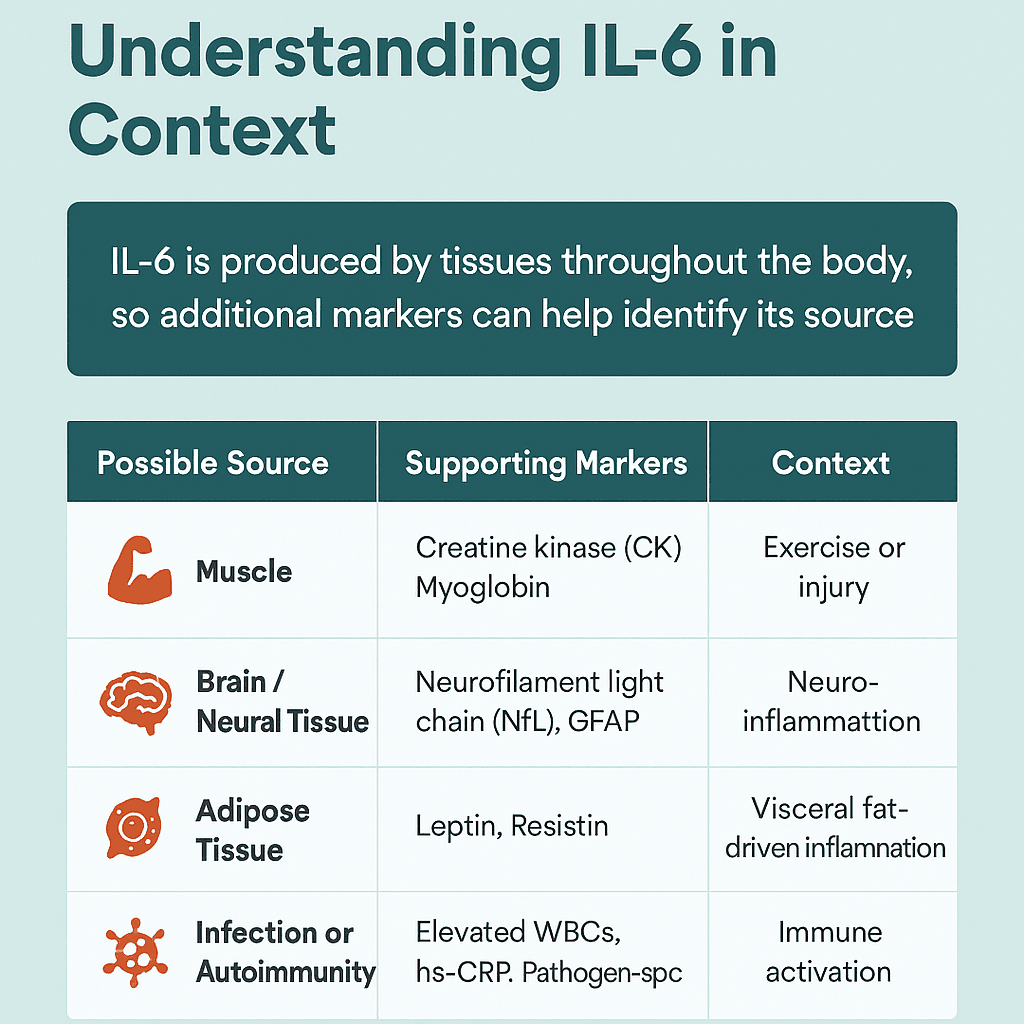
In these cases, pairing IL-6 with co-markers can help localize the source
In this case, pairing IL-6 with targeted co-markers helps you narrow down the source:
| Possible Source | Supporting Co-Markers | What It Suggests |
|---|---|---|
| Adipose Tissue (Fat) | Leptin, Adiponectin (↓), Resistin | Visceral fat-driven inflammation, insulin resistance |
| Skeletal Muscle | Creatine kinase (CK), Myoglobin | Muscle stress or damage (exercise, injury) |
| Brain / Neural Tissue | Neurofilament light chain (NfL), GFAP | Neuroinflammation or early neurodegeneration |
| Chronic Infection | Elevated WBCs, hs-CRP + IL-6, Pathogen-specific IgGs | Low-grade or persistent immune activation |
| Autoimmune Activation | IL-6 + ANA, RF, or anti-dsDNA | Potential early-stage autoimmune signaling |
CRP elevated + IL-6 normal:
But what if your IL-6 level is normal and CRP is still elevated?
When hs-CRP is mildly elevated but IL-6 remains within interleukin 6 normal range, it can suggest residual low-grade inflammation or inflammatory activity driven by other immune pathways (TNF-α, and IL-1β).
In metabolic dysfunction or poor metabolic health (such as obesity, insulin resistance, or visceral adiposity), it’s can be the case that CRP will remain mildly elevated without a major IL-6 spike, because the inflammation is low-grade and ongoing rather than acute.
This distinction can help you narrow in on whether interventions are necessary—or whether gradual metabolic optimization is the appropriate focus.
Normal CRP: Does the IL-6 Level Still Matter?
One of the biggest myths in inflammation testing is this:
“Normal CRP means you’re in the clear.”
It doesn’t.
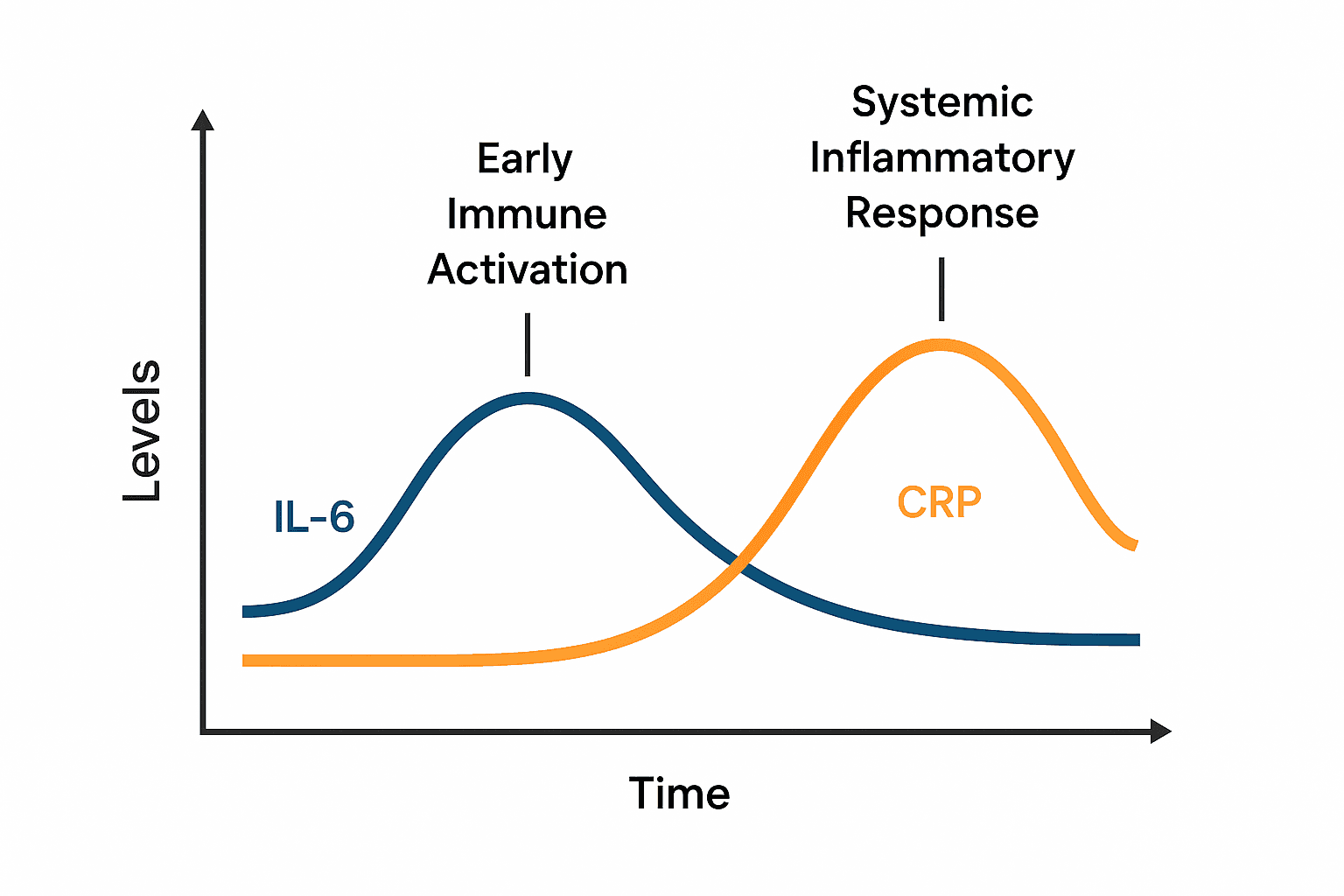
CRP is a downstream responder—slow to rise, slow to fall.
But IL-6 is the upstream messenger—and it often elevates long before CRP does.
IL-6 levels can be elevated even when CRP is perfectly normal—and this early rise has been shown in major studies to predict cardiovascular events and neurodegeneration independently of CRP levels.
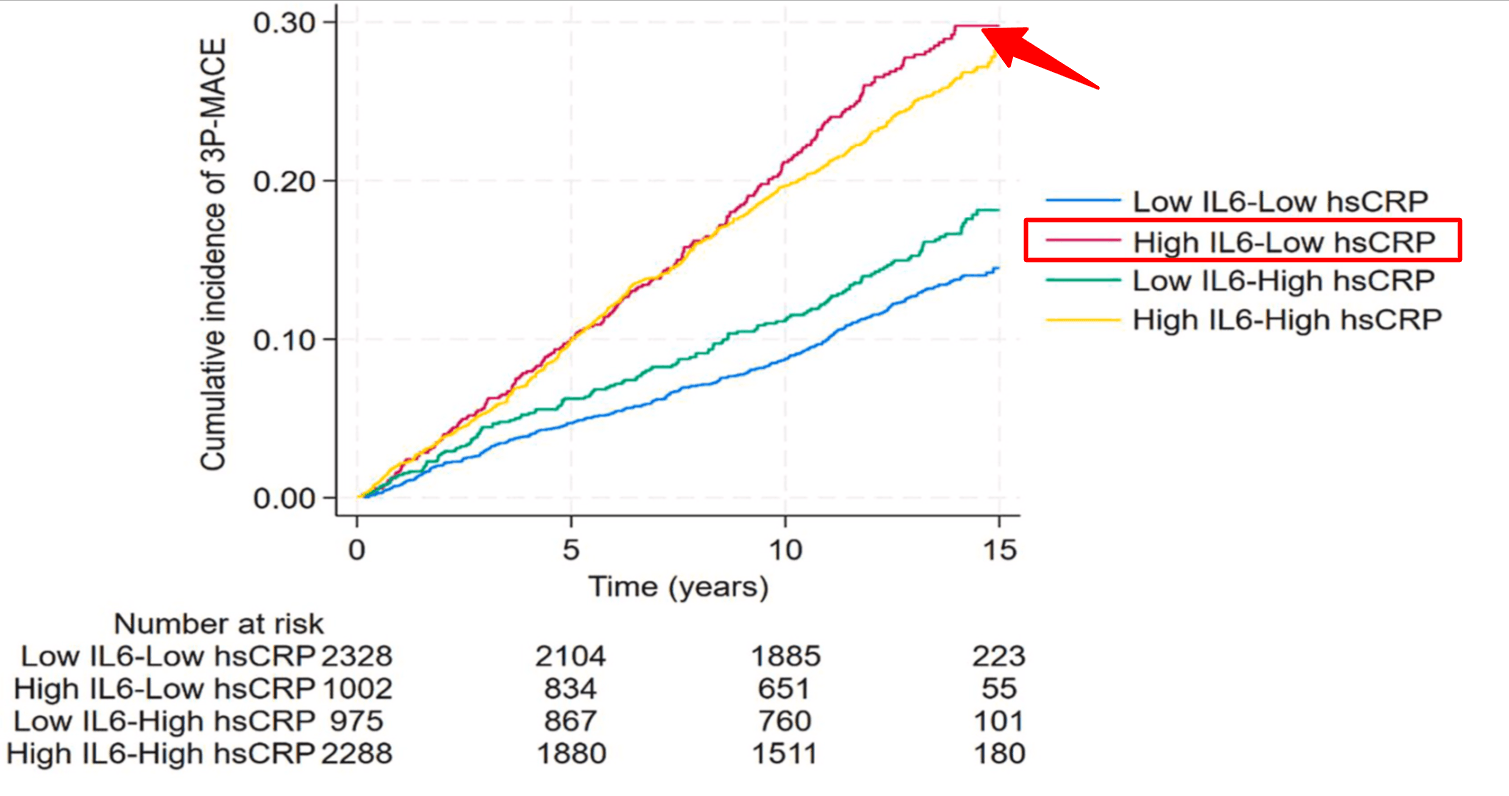
That’s why an interleukin 6 lab test is so useful for catching subtle, subclinical risk—especially if you have:
- Family history of cardiovascular disease, dementia, or autoimmune conditions
- Signs of visceral fat (high waist circumference, fatty liver, or metabolic syndrome)
- Early signs of metabolic issues (e.g., borderline fasting glucose, high normal triglycerides)
- Cognitive complaints—brain fog, memory lapses, or processing speed issues with no clear explanation
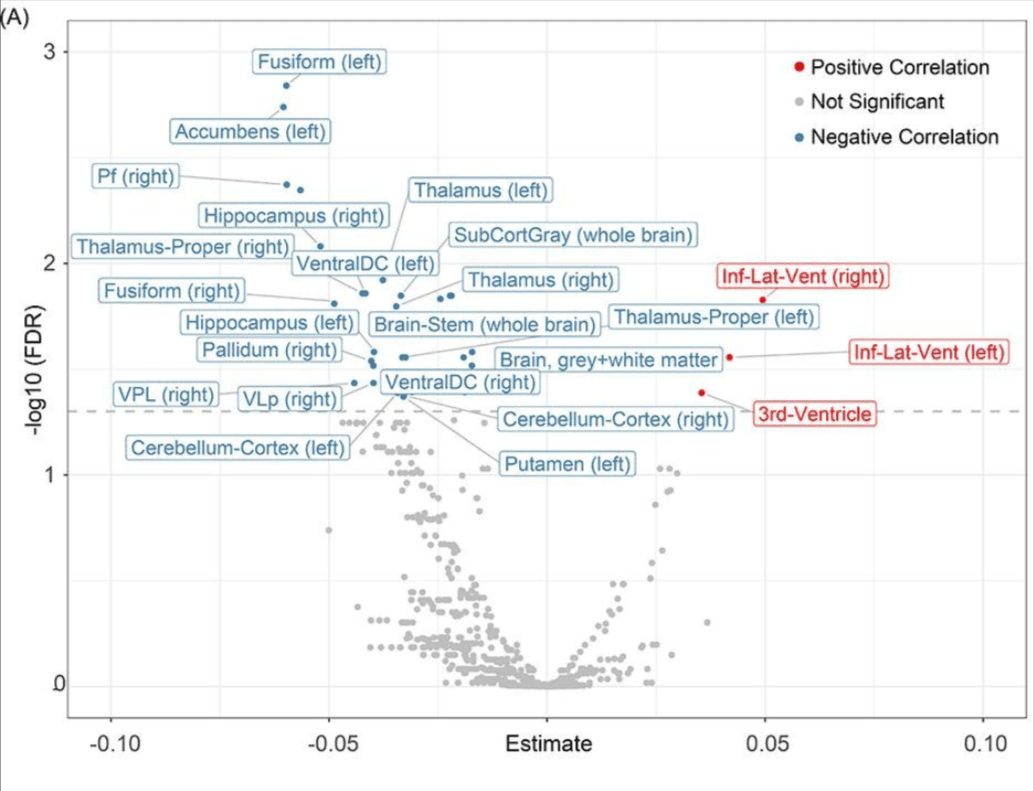
An elevated IL-6 level with a normal CRP could flag vascular, metabolic, or neuroinflammatory activity years before symptoms escalate—giving you a chance to intervene early. We previously covered IL-6’s relationship to brain health and inflammation in-depth. If you missed it, you can read it here.
Using An interleukin 6 lab test to Spot Early Autoimmune Inflammation: When Immune Symptoms Don’t Match the Labs
You feel like something’s off: fatigue, joint stiffness, gut issues. Maybe your family has a strong autoimmune history. But your labs come back “normal”—negative ANA, negative RF.
That doesn’t mean there’s no immune activity beneath the surface.
Autoimmunity doesn’t start overnight. Before adaptive immune dysfunction shows up on traditional panels, there’s usually a long smoldering phase of innate immune activation—and IL-6 is often the first to rise.
If your symptoms persist but standard autoimmune tests don’t show anything, this is where an IL-6 blood test can provide early clarity.
IL-6 can be especially helpful if:
- You have a family history of autoimmune disease
- You’ve experienced vague but recurring inflammation (fatigue, stiffness, gut flares)
- You want to intervene before damage occurs—not after a diagnosis is stamped
To be clear: IL-6 is not a diagnostic marker for autoimmune disease. But it can be the first signal that something’s brewing—long before tissue damage or serology turns positive.
That makes IL-6 potentially an underutilized tool in early immune detection.
Note: Autoimmune diseases are serious medical conditions that require diagnosis and treatment by a qualified healthcare professional. While IL-6 testing can offer early clues about immune activation, it is not a diagnostic tool on its own. If you suspect autoimmune risk, use your IL-6 results as a conversation starter with your doctor—not a replacement for clinical evaluation.
How IL-6 Lab Test Can Inform What You Do
Most people measure inflammation reactively—once there’s already pain, swelling, or dysfunction.
The interleukin 6 lab test flips that on its head. It helps you identify problems before they manifest.
Here’s how an interleukin 6 lab test can help inform what you do:
- It identifies early immune activation: long before symptoms, before a flare, and before CRP moves
- It targets intervention: If IL-6 is elevated, you might look more closely at visceral fat, gut permeability, chronic infection markers, or autoimmune risk—not just general inflammation. And if you want to understand how IL-6 drives stubborn belly fat (even in lean bodies), this article breaks it down—with research on why fat loss resistance is often inflammatory, not caloric.
- It tracks impact: If you’re already on an anti-inflammatory protocol—like a diet shift, gut protocol, or methylation support—you’ll know if it’s working by watching IL-6 drop
In short: Interleukin 6 test (IL-6 test) turns guesswork into strategy.
If you’re optimizing for prevention—not just disease management—this is the kind of data that changes your decision-making.
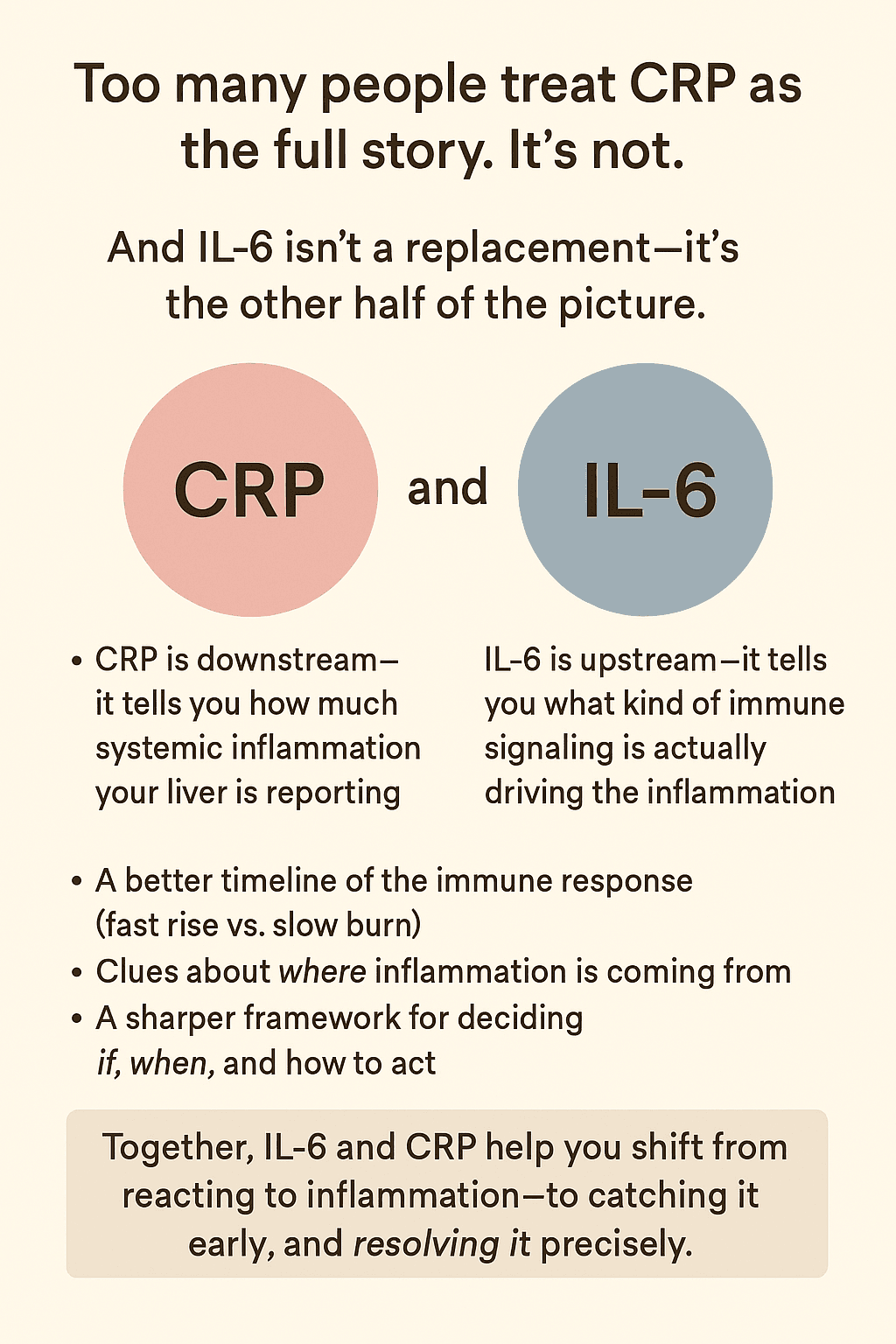
IL-6 and CRP Together: A More Complete Picture
Most people rely on CRP alone to track inflammation. It’s a familiar number.
But CRP only tells part of the story—and usually tells it late.
Think of CRP as your liver’s status report. It responds after the body has already been reacting. It tells you that inflammation has happened.
Get Weekly Insights to Personalize Your Own Longevity Roadmap
IL-6, on the other hand, is the message before the fire spreads.
It rises earlier, often from specific tissues, and signals that the immune system is already active—even if symptoms haven’t shown up yet.
That’s why testing both markers together doesn’t create redundancy—it creates a fuller picture:
- IL-6 gives you the first signal—what’s happening, where it might be coming from, and how active it is
- CRP shows the systemic burden—how the body is responding overall
When you test both, you get:
- A better timeline of the immune response (fast rise vs. slow burn)
- Clues about where inflammation is coming from
- A sharper framework for deciding if, when, and how to act
Together, IL-6 and CRP turn scattered immune signals into something actionable.
Not just a snapshot of inflammation—but a map for resolving it early and precisely
2. How I Personally Use IL-6 Testing for Longevity
Right now, my hs-CRP is <0.1 mg/L—below the detection threshold. That’s exactly where I want it for optimal aging.
But if it ever rose to the 1.0–2.0 mg/L range—and stayed there across two tests a month apart—I wouldn’t wait.
I’d ask my doctor for an IL-6 test. And if they declined? I’d order it myself through a specialty lab.
Why? Because even when CRP is “borderline normal,” IL-6 can already be rising. And persistent IL-6 elevation has been tied to:
- 42% higher risk of cognitive decline
- 25% greater risk of dementia
- Shrinking brain volume in subcortical regions
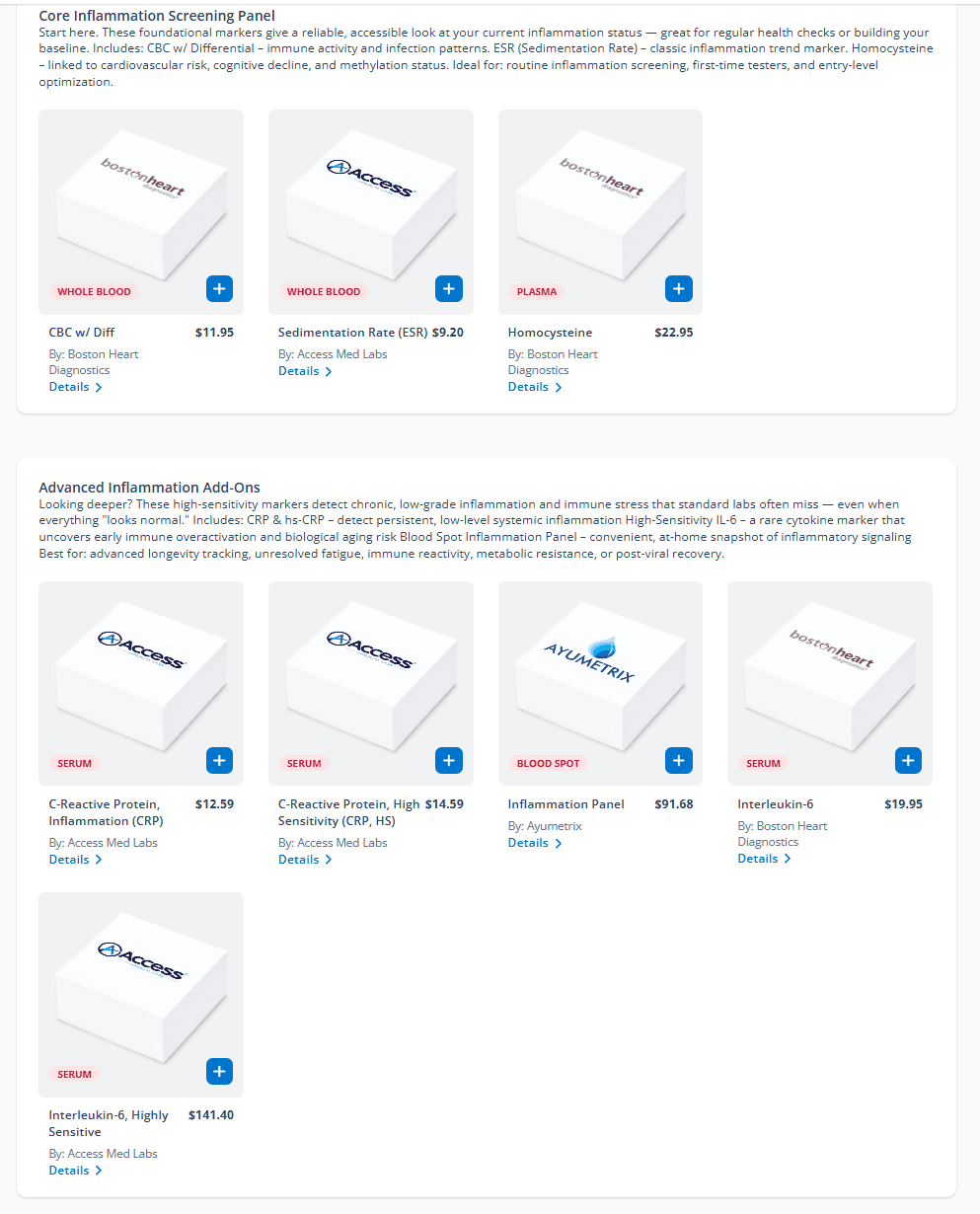
This is the exact test I would order if my CRP hit 1.5+
It’s the IL-6 test I recommend when everything else looks “normal.” Choose between standard IL-6 and high-sensitivity IL-6 (hs-IL-6) testing—and get the full picture early.
3. Interleukin 6 Normal Ranges: What IL-6 Levels Mean for Longevity
Understanding interleukin 6 test (IL-6 test) requires more nuance than simply flagging a “high” or “low” result. It’s important to understand both the reference ranges and the factors that can influence them.
Standard Reference Ranges for Interleukin 6 Test (IL-6 Test)
For healthy adults, IL-6 lab test results typically fall into the following lab ranges:
- Conventional IL-6 tests: Often define normal as <5–10 pg/mL, though exact cutoffs vary by lab.
- High-sensitivity IL-6 (hs-IL-6) tests: These more precise assays typically report a normal range of <1.5–2 pg/mL.
Because IL-6 rises early in the inflammatory process and clears quickly, a “snapshot” level can vary—but persistently low levels are generally associated with better health outcomes.
What Affects Your IL-6 Levels?
Even if your IL-6 test results are technically “normal,” they may not reflect your healthiest baseline. Several factors can impact what’s considered a normal IL-6 level:
- Circadian Rhythm: IL-6 tends to be lower in the morning and higher in the evening.
- Physical Activity: Regular exercisers typically have lower baseline IL-6. However, recent intense exercise can cause a temporary spike lasting 6–24 hours.
- Body Composition: Higher visceral fat correlates strongly with elevated IL-6 production, even in otherwise healthy individuals.
- Sex Differences: Hormonal fluctuations can slightly influence IL-6, although ranges largely overlap between men and women.
- Age: IL-6 levels tend to rise gradually with aging due to low-grade chronic inflammation. However, maintaining levels at the lower end of the range appears beneficial at any age.
IL-6 Levels: How to Read the Numbers
In clinical and functional medicine settings, IL-6 values are often interpreted along these lines:
- <1 pg/mL: Optimal, associated with minimal inflammatory burden
- 1–2 pg/mL: Normal, seen in most healthy adults
- 2–5 pg/mL: Mild elevation, potential low-grade inflammation
- 5–10 pg/mL: Moderate elevation, typically warrants further investigation
- >10 pg/mL: Markedly elevated, often seen in acute illness or chronic inflammatory conditions
Why IL-6 Levels Matter for Longevity
For those focused on inflammation and aging, “normal” isn’t always good enough. The long-term goal is to keep IL-6 as low as feasible without clinical suppression.
- <1 pg/mL is often considered an optimal target for anti-aging and brain preservation strategies.
- 1–2 pg/mL is acceptable and probably considered to be within interleukin 6 normal range but may warrant monitoring over time.
- >2 pg/mL, especially if persistent across multiple tests, without recent infection or intense training—may indicate the need for interventions (either ilifestyle of medical) aimed at reducing systemic inflammation.
One test is just a data point. Trend is everything. Tracking IL-6 over time gives you a window into how your interventions are working, and whether you’re staying ahead of age-related immune drift.
Here’s a quick reference table summarizing IL-6 ranges, what they mean clinically, and useful references for healthy aging:
| IL-6 Range (Interleuikin 6 Blood levels) | Details |
|---|---|
| Longevity Context | |
| Ideal target for longevity <1 pg/mL | |
| Acceptable for healthy aging 1–2 pg/mL | |
| May warrant intervention (if persistent) >2 pg/mL | |
| Conventional IL-6 Range | Generally considered normal if <5–10 pg/mL (varies by lab) |
| High-Sensitivity IL-6 (hs-IL-6) Range | Typically considered normal if <1.5–2 pg/mL |
| Time of Day Effect | Lower in morning, higher in evening |
| Physical Activity Effect | Lower baseline in regular exercisers; temporary spikes post-exercise |
| Body Composition Effect | Higher with greater body fat, especially visceral fat |
| Sex Differences | Minor differences; hormonal influences may affect levels slightly |
| Clinical Context | |
| Optimal (minimal inflammatory burden) <1 pg/mL | |
| Within interleukin 6 normal range for most healthy adults 1–2 pg/mL | |
| Mildly elevated (possible low-grade inflammation) 2–5 pg/mL | |
| Moderately elevated (higher inflammatory activity) 5–10 pg/mL | |
| Markedly elevated (acute disease state likely) >10 pg/mL |
4. Practical Considerations for IL-6 Testing
Differentiating Sources of IL-6
When IL-6 levels are elevated, the key question isn’t just “how much”—it’s why.
Because IL-6 is produced in response to many stressors—immune activation, tissue damage, metabolic dysfunction—the surrounding context helps pinpoint the source.
That doesn’t make IL-6 hard to interpret. It makes it directional—as long as you know what patterns to look for.
Pattern Recognition: What Cytokine Signatures Can Reveal about IL-6 Inflammaion
Different types of inflammation leave different fingerprints in the immune system.
- Exercise-induced IL-6 Inflammaion is typically isolated—it rises quickly and resolves fast, with no elevation in TNF-α or IL-1β.
- Infection-related IL-6 Inflammaion usually occurs with TNF-α, IL-1β, and sometimes elevated WBCs.
- Autoimmune activation may show a persistent IL-6 elevation alongside markers like ANA, RF, or other adaptive immune indicators.
- Adipose-driven IL-6 Inflammaion may include IL-6, hs-CRP, and shifts in leptin/adiponectin ratios—but again, without other acute-phase cytokines.
By mapping which markers rise together—and which don’t—you can start to infer which systems are active.
IL-6 isn’t a vague signal. It’s a clue in a larger immune dialogue.
When viewed alongside timing, symptoms, and companion markers, it becomes a map—not a mystery.
How Exercise Affects IL-6 Levels in Your Interleukin 6 Lab Test (IL-6 Lab Test)
IL-6 levels spiking after workouts have caused confusion—even in clinical settings. Here’s how to make sense of it.
IL-6 Levels Can Surge After Exercise—and That’s OK
During moderate or intense training, your muscle fibers release IL-6—sometimes up to 100x your baseline.
- This surge isn’t a sign of damage.
- It’s part of how your body signals for glucose uptake, fat burning, and recovery.
Levels usually return to baseline within 6–24 hours.
The Key Distinction: Myokine vs. Inflammatory Signal
When muscle releases IL-6, it acts as a myokine—a metabolic messenger that supports health.
That’s very different from IL-6 inflammation triggered by infection or chronic immune stress, which tends to linger and signal tissue dysfunction.
Knowing which type of IL-6 inflammation you’re dealing with is everything.
Best Practices for Accurate IL-6 Lab Testing
To get meaningful interleukin 6 test results:
- Avoid training for 24–48 hours before the blood draw.
- Schedule your interleukin 6 lab test in the morning, ideally after a rest day.
- Repeat under similar conditions if you’re monitoring trends.
IL-6 is a fast responder. But its speed can also make it vulnerable to misinterpretation—unless your testing setup is consistent.
Not sure how to fix your high normal CRP?
CRP tells you there’s inflammation. IL-6 helps you figure out where it’s coming from. Choose from standard or high-sensitivity IL-6 testing to match your level of risk and tracking goals.
FAQ
What is the normal range for IL-6?
Normal IL-6 ranges vary by test type, but <5 pg/mL is typical; <1.5 pg/mL is ideal on high-sensitivity tests.
Conventional IL-6 tests often use <5–10 pg/mL as the upper limit. High-sensitivity IL-6 (hs-IL-6) tests define optimal as <1.5–2 pg/mL. From a longevity standpoint, <1 pg/mL is considered a target for minimal inflammation. Always interpret in context—timing, lifestyle, and co-markers matter.
What does elevated interleukin-6 mean?
Elevated IL-6 means active inflammation—potentially driven by fat, infection, stress, or early autoimmune activity.
Because IL-6 rises early in the immune cascade, it may flag issues long before CRP, ESR, or symptoms appear. Persistent elevations (even if mild) suggest chronic immune stimulation. This could point to visceral fat, blood sugar dysregulation, gut inflammation, or hidden infection—each requiring different strategies.
→ In our Deep Inflammation Panel, you can test IL-6 alongside CRP, ESR, WBCs, and more—then select the markers that best match your health goals and what you have recently been tested for.
How do you treat high IL-6 levels?
Treating high IL-6 starts with identifying the cause—then targeting it through lifestyle, anti-inflammatory support, or clinical care.
Interventions depend on context: visceral fat, metabolic stress, or gut issues may all drive IL-6. Reduce sugar and seed oils, optimize sleep, use recovery-focused training, and consider supplements like omega-3s, curcumin, or quercetin. Serial testing helps confirm if changes are working.
How to reduce IL-6 naturally?
You can lower IL-6 naturally with anti-inflammatory foods, stress management, sleep, and exercise—when done right.
Cut ultra-processed foods, prioritize omega-3s and polyphenols, and keep blood sugar stable. Prioritize consistent, moderate-intensity movement and adequate sleep. Breathwork, sauna, and gut support may also reduce IL-6 levels over time. Retest after 6–12 weeks to track change.
Does IL-6 increase with age?
Yes, IL-6 tends to rise with age, contributing to “inflammaging” and age-related disease risk.
This rise isn’t just passive—it’s often linked to increased visceral fat, declining mitochondrial function, and immune dysregulation. Higher IL-6 is associated with frailty, cognitive decline, cardiovascular disease, and reduced resilience. Monitoring and controlling IL-6 is key to aging well.
What triggers IL-6 release?
IL-6 is triggered by infection, injury, metabolic stress, and inflammation—especially from visceral fat or immune activation.
It’s also produced during intense exercise (temporarily) and psychological stress. Chronic triggers include poor diet, gut issues, poor sleep, and unresolved infections. Understanding the source of IL-6 can guide your approach—whether you need rest, detox, or deeper testing.
Is high IL-6 bad?
High IL-6 isn’t always bad—but persistent elevation is a red flag for chronic inflammation and future disease.
Temporary spikes after exercise are normal. But if IL-6 remains elevated at rest—especially alongside fatigue, brain fog, or CRP—it could signal metabolic dysfunction, neuroinflammation, or immune stress. The earlier you detect it, the easier it is to reverse.
What is the main source of IL-6?
IL-6 is produced by immune cells, fat tissue, muscle, the brain, and gut—depending on the trigger.
In obesity and aging, visceral fat becomes a key source. During infection, immune cells flood the bloodstream with IL-6. Exercise triggers temporary spikes from muscle. Neuroinflammation and gut dysbiosis can also contribute. Testing helps determine which pathway is active.
What is the best time to test IL-6?
Test IL-6 in the morning, ideally after 24–48 hours without intense exercise or illness.
IL-6 follows a diurnal rhythm—lowest in the morning and higher in the evening. It also spikes after training or acute stress. To get a meaningful baseline, fast overnight, skip intense workouts for two days, and avoid recent infections or flares before testing.
📈 Conclusion: Why an Interleukin 6 Test (IL-6 Test) Adds Early Clarity to Inflammation Detection
Bottom line: If you’re only testing CRP, you’re catching the aftermath.
If you include an interleukin 6 test, you see the signal before the fire spreads.
Research shows the interleukin 6 lab test predicts cardiovascular events even when hs-CRP is low—a clear sign that we’re often missing early immune risk in people who otherwise “look fine” on labs (PMC). In a study involving 14 916 apparently healthy men, elevated levels of IL-6 were associated with increased risk of myocardial infarction (Pubmed).
What sets IL-6 apart?
It rises faster. Clears faster. And offers tissue-specific, pathway-targeted information you won’t get from CRP alone. From brain inflammation and cognitive decline to metabolic dysfunction and aging, IL-6 doesn’t just show what’s happening—it often points to what’s coming.
Meanwhile, CRP and hs-CRP remain valuable tools for tracking the overall burden of inflammation. But on its own, it can miss the signal upstream.
For anyone serious about prevention, brain health, or optimizing for longevity, testing both IL-6 and CRP provides a clearer timeline, better insight, and faster feedback on whether your strategies are working.
IL-6 doesn’t replace CRP.
It completes the picture.
And that’s what turns a blood test into a precision tool for longevity.
🧪 Build Your Personalized Inflammation Panel
Track what your CRP can’t. Choose from standard or high-sensitivity IL-6 tests, plus essential co-markers like hs-CRP, ESR, and Homocysteine.
Whether you’re optimizing for brain health, reversing hidden inflammation, or fine-tuning your longevity strategy—this is where clarity starts
References
- Ridker PM, Rifai N, Stampfer MJ, Hennekens CH. Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation. 2000 Apr 18;101(15):1767-72. doi: 10.1161/01.cir.101.15.1767. PMID: 10769275.
- Mehta NN, deGoma E, Shapiro MD. IL-6 and Cardiovascular Risk: A Narrative Review. Curr Atheroscler Rep. 2024 Nov 26;27(1):12. doi: 10.1007/s11883-024-01259-7. PMID: 39589436; PMCID: PMC11599326.
- Bradburn S, Sarginson J, Murgatroyd CA. Association of Peripheral Interleukin-6 with Global Cognitive Decline in Non-demented Adults: A Meta-Analysis of Prospective Studies. Front Aging Neurosci. 2018 Jan 8;9:438. doi: 10.3389/fnagi.2017.00438. PMID: 29358917; PMCID: PMC5766662
- Ferreira JP, Vasques-Nóvoa F, Neves JS, Zannad F, Leite-Moreira A. Comparison of interleukin-6 and high-sensitivity C-reactive protein for cardiovascular risk assessment: Findings from the MESA study. Atherosclerosis. 2024 Mar;390:117461. doi: 10.1016/j.atherosclerosis.2024.117461. Epub 2024 Jan 24. PMID: 38306764.
- Puzianowska-Kuźnicka M, Owczarz M, Wieczorowska-Tobis K, Nadrowski P, Chudek J, Slusarczyk P, Skalska A, Jonas M, Franek E, Mossakowska M. Interleukin-6 and C-reactive protein, successful aging, and mortality: the PolSenior study. Immun Ageing. 2016 Jun 3;13:21. doi: 10.1186/s12979-016-0076-x. PMID: 27274758; PMCID: PMC4891873.