When we talk about aging, most people think of grey hair, wrinkles, or maybe a slower metabolism.
But in men, two of the earliest signs of biological stress show up in systems that are rarely viewed through a longevity lens: testosterone levels and sperm health.
These aren’t just fertility metrics.
They’re early indicators of how your body handles inflammation, repair, and energy production. And while few doctors will mention it, vitamin B12 and male fertility are closely connected – and Vitamin B12 sits upstream of many of these processes.
Sperm DNA health predicts more than offspring outcomes. It reflects your own aging trajectory.
Low B12 doesn’t just cause fatigue or brain fog. It can disrupt hormone balance, increase oxidative stress, and impair DNA stability.
And sperm, with their intense energy needs and minimal DNA repair capacity, are often the first to show the damage—making vitamin B12 and fertility an overlooked link.
This article breaks down three early signs of aging in men—testosterone decline, reduced sperm motility, and sperm DNA fragmentation—and why vitamin B12 status may be the missing link.
Table of Contents
Vitamin B12 and Testosterone – The First System to Strain
Before you notice low energy or fading libido, testosterone has already started reflecting deeper dysfunction.
It’s more than a sex hormone—it’s an early signal of how well your body handles internal stress.
If B12 drops, testosterone is often the first to fall—but rarely the last.
Testosterone depends on three key systems: mitochondrial function, nitric oxide signaling, and methylation efficiency—all supported by vitamin B12.
So when B12 drops, testosterone is often one of the first to follow.
It’s not that B12 directly “boosts” testosterone.
What it does is keep the systems that sustain testosterone working: cellular energy production, nitric oxide signaling, and detoxification of homocysteine—an inflammatory compound that rises when B12 is deficient.
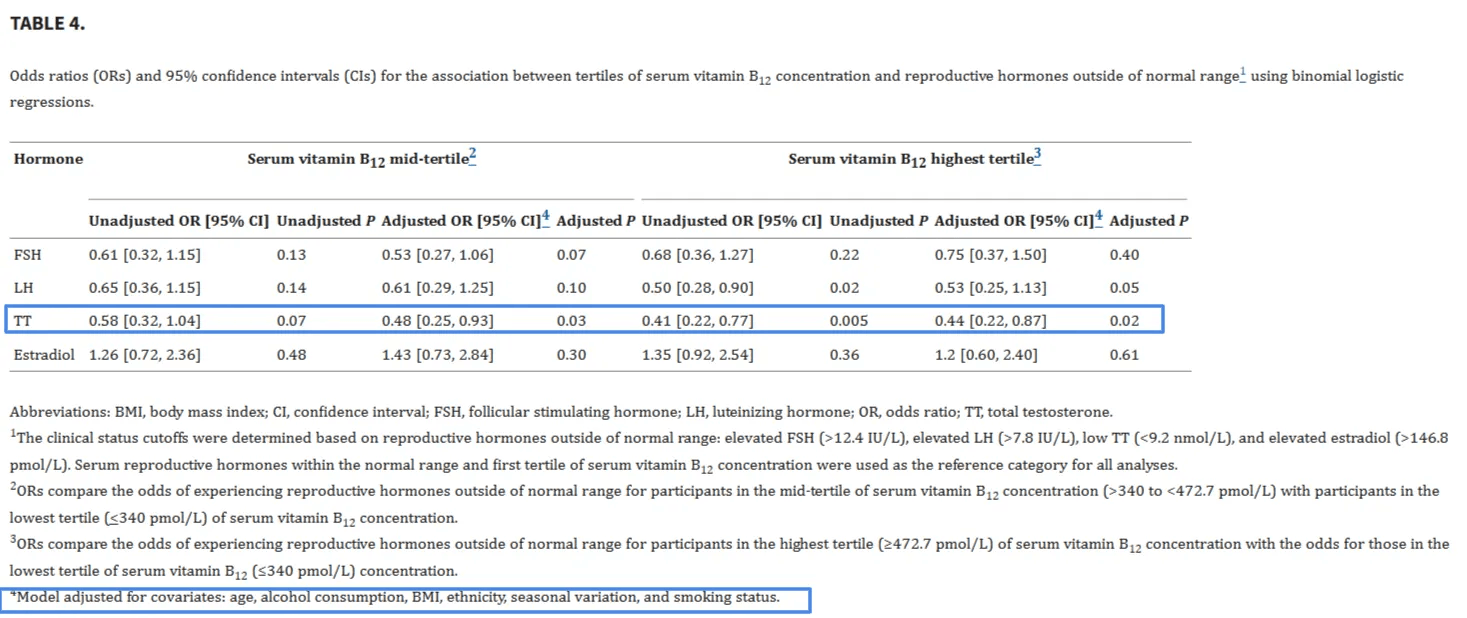
A 2024 study from Mount Sinai Hospital found an independent link between vitamin B12 and testosterone in men with infertility.
Researchers analyzed 303 men and found that those in the lowest third of B12 levels had 127% higher odds of testosterone deficiency compared to those in the highest third—even after adjusting for age, BMI, alcohol, smoking, ethnicity, and season (Rastegar, 2024). In other words, the association between B12 and testosterone held steady regardless of these other common influences.
Among men with infertility, low serum vitamin B12 is associated with a higher risk of testosterone deficiency and impaired androgenic hormonal profiles that impact spermatogenesis and, consequently, fertility.
Rastegar, 2024
Low testosterone isn’t the cause—it’s a downstream marker.
In many men, it’s one of the earliest detectable signs of disrupted methylation and mitochondrial function—if it’s tested.
Vitamin B12 and Sperm Motility: Sperm Quality as a Cellular Aging Marker
Sperm: your most sensitive aging biomarker?
Sperm are high-performance cells. They need speed, power, precision—and constant repair. That makes them unusually sensitive to subtle metabolic decline. In fact, sperm may be one of the first cell types in your body to reflect biological aging.
Changes in sperm quality—like count, motility, and morphology—can reveal early dysfunction in systems that maintain cellular energy, antioxidant defense, and DNA stability.
It’s part of why vitamin B12 and sperm, sperm quality deserve more attention in longevity science—not just in fertility clinics.
We’ve known this for decades.
In a 1984 trial, methylcobalamin was given to 26 infertile men for 4 to 24 weeks. Depending on the parameter measured—sperm concentration, motility, or total motile count—38–54% of patients showed improvement. By the study’s overall clinical criteria, 42% were classified as responders (Isoyama, 1984). And that was before we understood oxidative stress and DNA repair the way we do today.
Today, we know much more about the mechanisms. A 2017 review identified multiple studies showing that low B12 correlates with elevated homocysteine, impaired nitric oxide signaling, and increased oxidative damage to sperm—all of which impair motility and morphology.
We don’t usually think of sperm as aging biomarkers—but maybe we should.
Multiple human trials using doses between 1500 and 6000 µg/day have shown improvements in sperm count and motility (Banihani, 2017). These effects reflect B12’s role in reducing oxidative stress and supporting a more stable biochemical environment for sperm. This is central to both vitamin B12 and sperm motility, physiology and the broader conversation on vitamin B12 and fertility.
To sum it up: sperm quality reflects systemic stress. And B12 appears to shield these cells from the early cracks—oxidative load, low methylation potential, and impaired signaling.
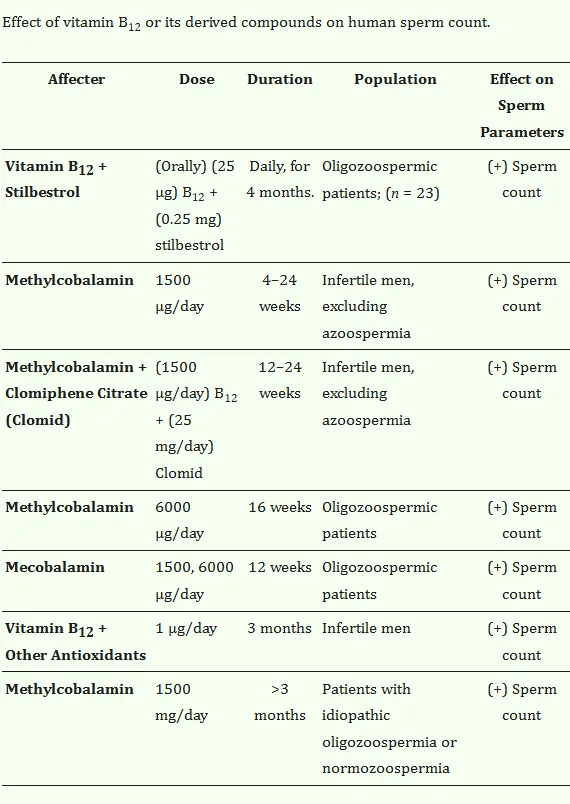
This table summarizes findings from several human trials—ranging from basic antioxidant support to targeted treatment for oligozoospermia (low sperm count). Across studies, B12 improved sperm count.
Vitamin B12 and Fertility – Sperm DNA Integrity as a Genomic Aging Signal
A 2015 study found that infertile men with varicocele—a common condition where swollen veins in the scrotum interfere with sperm production—who took a multivitamin including vitamin B12 for 3 months had a 22.1% reduction in sperm DNA fragmentation.
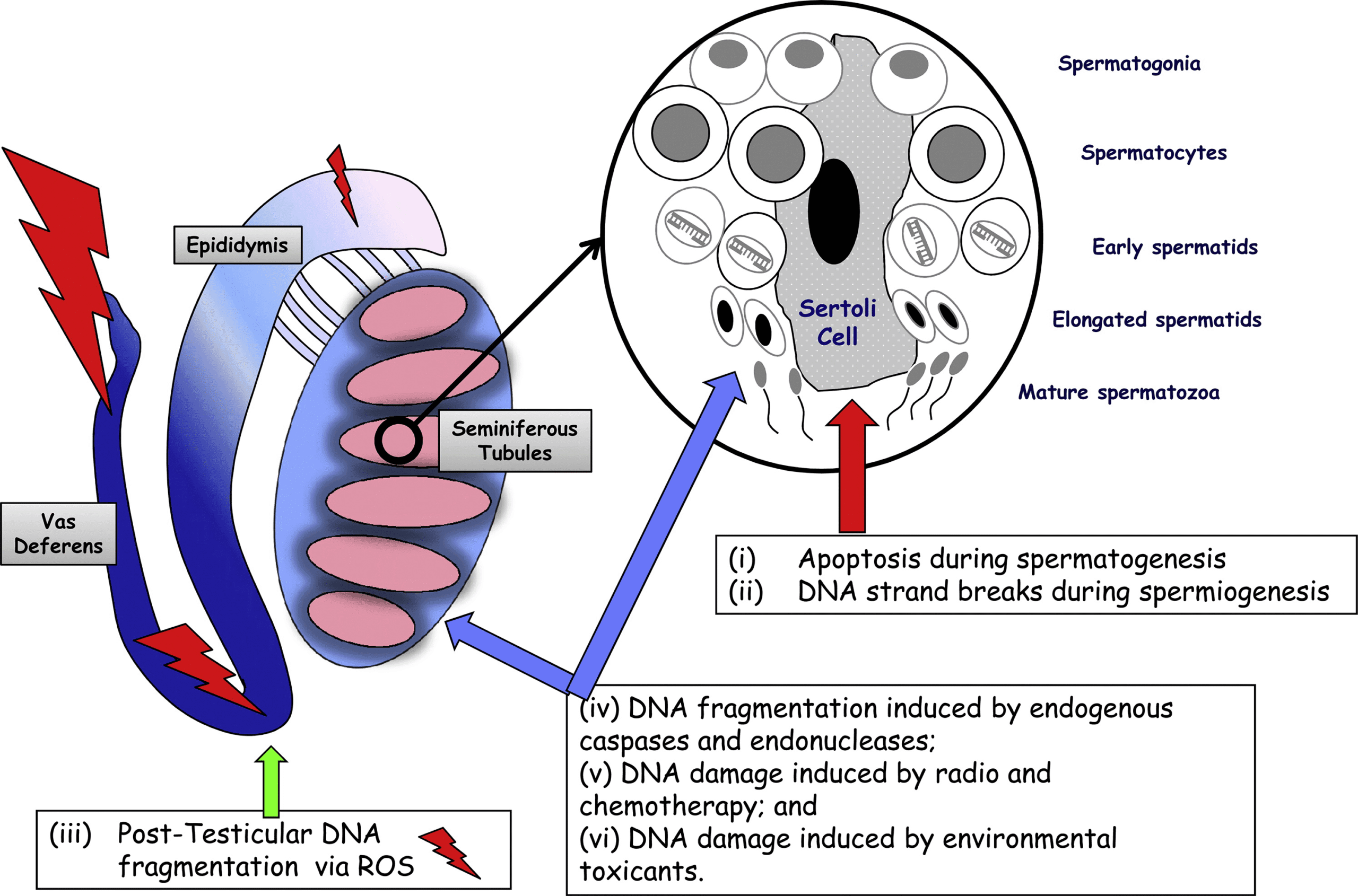
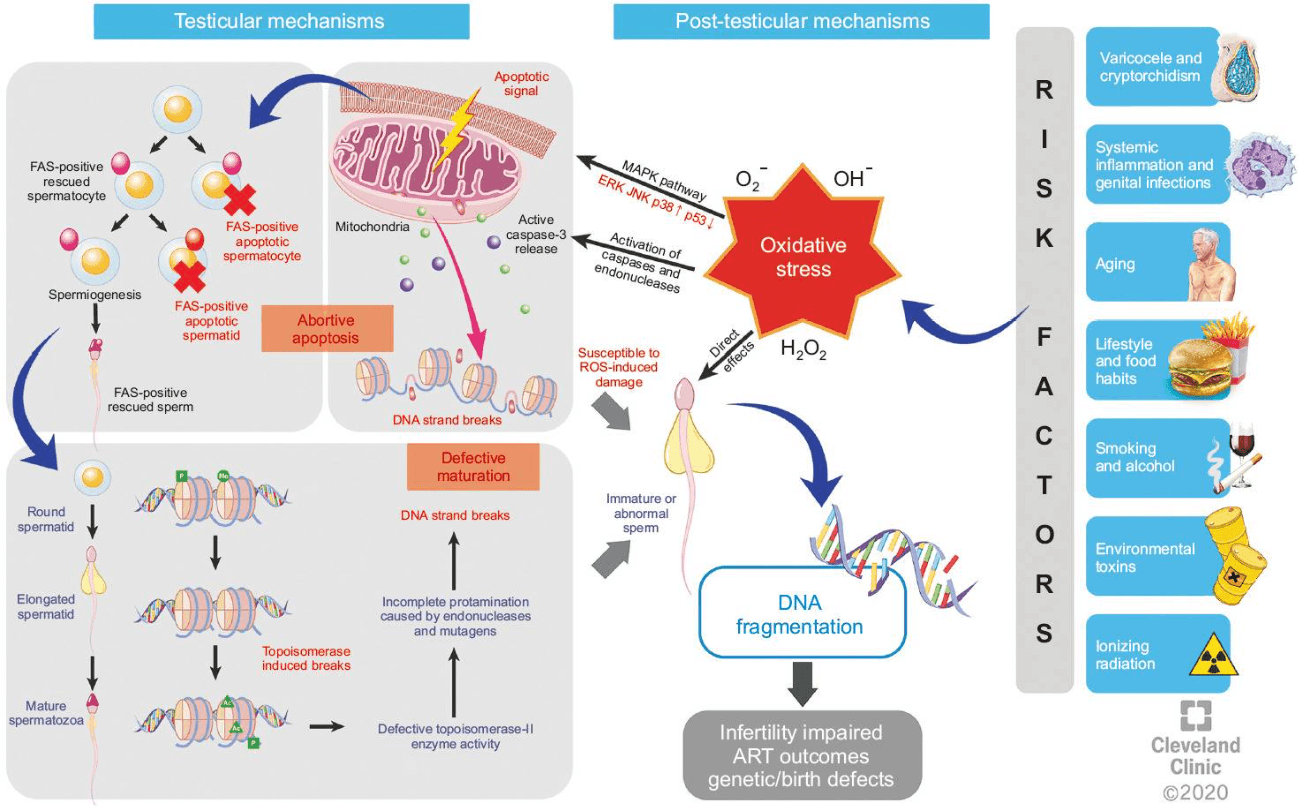
Elevated DNA fragmentation is a major contributor to male infertility—and often goes undetected by basic semen analysis. In fact, up to 25–40% of infertile men with normal semen parameters have elevated levels of sperm DNA fragmentation.
Sperm DNA fragmentation refers to breaks or damage in the genetic material carried by sperm. Unlike structural issues like morphology or motility, fragmentation affects the genome itself—impacting fertilization, embryo quality, and potentially long-term offspring health.
Sperm are vulnerable.
Once mature, they lose most of their DNA repair capacity. That means oxidative stress, methylation errors, or nutrient deficiencies—especially low B12—can directly compromise DNA integrity. And because sperm production relies on rapid replication under tight resource constraints, they can be one of the the first systems to show molecular signs of strain.
Vitamin B12 supports methionine synthase, a key enzyme in the methylation cycle that stabilizes DNA and ensures proper chromatin packaging (one of the ways the link between vitamin B12 and fertility plays out at the molecular level.)
As mentioned in our prior article, vitamin B12 also buffers homocysteine, a metabolite that promotes oxidative damage and impairs nitric oxide signaling. When B12 is low, homocysteine rises, glutathione reserves drop, and reactive oxygen species (ROS) accumulate—particularly in high-turnover tissues like the testes (Banihani, 2017).
The result is early fragmentation of sperm DNA and weakened chromatin structure.
Notably in both clinical and lab models, B12 supplementation reduces this damage.
For example, in a cryopreservation study, sperm samples exposed to 2 mg/mL of vitamin B12 had significantly better post-thaw viability and lower DNA fragmentation than untreated controls (Hosseinabadi, 2020). Other concentrations (1–2 mg/mL) also improved motility and antioxidant responses.
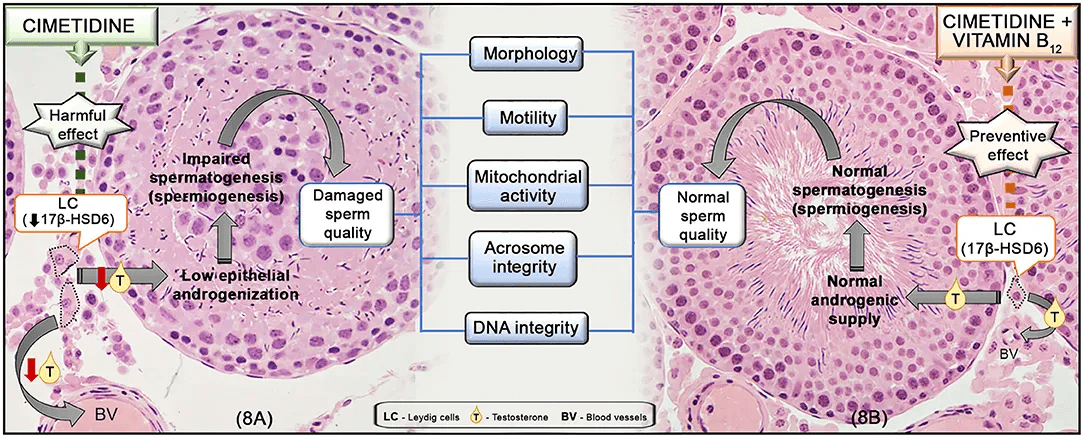
Animal studies show similar results. In a 2019 experiment, rats exposed to the androgen-disrupting drug cimetidine showed impaired sperm quality—unless they received vitamin B12. With B12 treatment, their DNA integrity, motility, and morphology remained intact (Beltrame, 2019). These molecular processes underpin the broader links between vitamin B12 and fertility and vitamin B12 and testosterone.
📋 Test Vitamin B12 and Testosterone
Want to catch early signs of decline tied to vitamin B12 and fertility or vitamin B12 and testosterone? These markers reveal patterns in nutrient metabolism, hormone balance, and genomic stress:
- Total B12
- Methylmalonic acid (MMA)
- Homocysteine
- Free testosterone, bioavailable testosterone and SHBG(for a full picture of active hormone levels)
What to Test for Vitamin B12 and Fertility, B12 and Testosterone, and Male Hormone Health
The patterns we’ve covered—low testosterone, declining sperm quality, DNA fragmentation—often begin with subtle shifts in nutrient metabolism.
These early shifts often show up in blood work, but their connection to sperm health and hormone balance is rarely recognized.
Holotranscobalamin (holoTC) is the most sensitive marker for early B12 deficiency. But since most labs don’t offer it, the next best option is to combine more accessible markers that reveal functional strain.
These are the key biomarkers to look for:
- Total B12: Helpful as a baseline, but can appear normal even when deeper problems exist.
- Methylmalonic acid (MMA): Rises when B12 isn’t functioning well inside cells.
- Homocysteine: A key marker in the vitamin b12 and fertility equation. Elevated levels impair methylation, fuel oxidative stress, and are linked to sperm motility, embryo quality, and DNA fragmentation.
- Free testosterone and SHBG: Together, these clarify how much bioavailable testosterone is circulating—not just the total. Bioavailable testosterone is calculated from free T and albumin-bound T, and reflects the active, usable hormone. Our panel includes this option for more accurate hormone assessment.
FAQ: How Vitamin B12 Affects Male Fertility, Testosterone, and Sperm Health
Does B12 increase testosterone?
Vitamin B12 may help maintain healthy testosterone levels by supporting nitric oxide signaling, energy metabolism, and methylation.
While vitamin B12 doesn’t directly stimulate testosterone production, it supports the systems that regulate it. Low B12 can disrupt nitric oxide synthesis and mitochondrial energy output—both essential for hormone signaling. Several studies show a correlation between vitamin B12 and testosterone levels, especially in men with deficiency or infertility.
Can B12 affect fertility?
Yes, vitamin B12 plays a key role in male fertility by protecting sperm DNA, improving motility, and supporting hormone regulation.
Research shows that vitamin B12 and fertility are closely linked. B12 supports methylation and reduces oxidative stress, both of which are essential for healthy sperm development. Deficiency has been associated with reduced sperm count, abnormal morphology, and impaired fertilization potential—even in men with otherwise normal hormone levels.
Does B12 help with sperm?
Vitamin B12 improves sperm motility, count, and DNA stability—especially in men with low or borderline levels.
Clinical studies show that vitamin B12 and sperm health are connected across multiple parameters. B12 supports mitochondrial activity in sperm cells, helps preserve DNA integrity, and enhances overall motility. Trials using methylcobalamin show measurable improvements in sperm count and motility within weeks of supplementation.
Can you take B12 and testosterone together?
Research suggests it is generally safe to take vitamin B12 and testosterone together, with no known interactions and potential benefits.
Vitamin B12 is involved in homocysteine metabolism and methylation—processes that are essential for testosterone synthesis and function. While B12 isn’t a replacement for testosterone therapy, taking them together can help optimize hormone metabolism. Some research links b12 and testosterone indirectly through shared pathways.
The evidence leans toward no additional side effects when taken together, but controversy exists around optimal dosages and long-term effects. For practical application, always consult a healthcare provider to ensure safety and efficacy.
What are the benefits of vitamin B12 for men?
Vitamin B12 supports energy, cognition, fertility, testosterone regulation, and long-term DNA integrity in men.
The benefits of vitamin B12 for men go beyond energy. It helps sustain healthy testosterone levels, supports sperm motility, improves DNA methylation, and protects against oxidative stress. These effects make B12 a key micronutrient for aging, fertility, and metabolic resilience.
What’s the difference between total, free, and bioavailable testosterone?
Total testosterone includes all testosterone in your blood—both active and inactive. But most of it is bound to proteins like SHBG and can’t be used by your cells.
Free testosterone is the small fraction that’s unbound and fully active.
Bioavailable testosterone includes both free testosterone and the portion loosely bound to albumin—this is what your body can actually use.
That’s why we include free testosterone, bioavailable testosterone, and SHBG in our panel. Together, they give a more accurate view of your hormone status than total testosterone alone.
Which vitamins increase testosterone?
Vitamin D, zinc, magnesium, and B12 can all support testosterone indirectly through nutrient-sensitive pathways.
While no vitamin is a direct testosterone booster, several—including vitamin B12—help maintain the conditions that allow testosterone production to function efficiently. B12’s role in nitric oxide generation and methylation supports both testosterone and sperm health, particularly in aging or nutrient-deficient men.
How does B12 deficiency affect sperm DNA?
Low B12 increases DNA fragmentation in sperm by impairing methylation and raising oxidative stress.
B12 helps regulate homocysteine and supports glutathione—two key defenses against DNA damage. In multiple studies, men with low B12 showed higher levels of sperm DNA fragmentation, even with normal hormone levels. This highlights the link between vitamin B12 and sperm motility, DNA integrity, and embryo quality.
Conclusion: Vitamin B12 and Male Fertility Matter Beyond Reproduction
Sperm quality and hormone levels aren’t just about reproduction—they reflect how fast you’re aging. DNA breaks, sluggish testosterone, and poor methylation are signs that your body’s repair systems are under strain.
Vitamin B12 is central to these processes. It supports hormone signaling, stabilizes methylation, and protects genomic integrity—linking vitamin B12 and fertility to much more than reproduction alone.
And it’s one of the easiest systems to test and improve.
📖 Want to go deeper?
- Understanding B12 test results: Learn how to interpret total B12, MMA, and homocysteine—even if your lab doesn’t include holoTC. → Read: How to Understand Your B12 Lab Results the Right Way
- Cognitive aging & B12: Explore how early B12 decline affects brain aging, methylation, and long-term memory resilience. → Read: Vitamin B12 and Brain Fog – What Blood Tests Miss About Early Cognitive Decline
B12 isn’t just a vitamin. It’s a genomic safeguard.
References
- Rastegar Panah M, Jarvi K, Lo K, El-Sohemy A. Vitamin B12 Is Associated with Higher Serum Testosterone Concentrations and Improved Androgenic Profiles Among Men with Infertility. J Nutr. 2024 Sep;154(9):2680-2687. doi: 10.1016/j.tjnut.2024.06.013. Epub 2024 Jun 26. PMID: 38936552; PMCID: PMC11393164.
- Banihani SA. Vitamin B12 and Semen Quality. Biomolecules. 2017 Jun 9;7(2):42. doi: 10.3390/biom7020042. PMID: 28598359; PMCID: PMC5485731.
- Beltrame FL, de Santi F, Vendramini V, Cabral REL, Miraglia SM, Cerri PS, Sasso-Cerri E. Vitamin B12 Prevents Cimetidine-Induced Androgenic Failure and Damage to Sperm Quality in Rats. Front Endocrinol (Lausanne). 2019 Jul 10;10:309. doi: 10.3389/fendo.2019.00309. PMID: 31354617; PMCID: PMC6635670.
- Hosseinabadi F, Jenabi M, Ghafarizadeh AA, Yazdanikhah S. The effect of vitamin B12 supplement on post-thaw motility, viability and DNA damage of human sperm. Andrologia. 2020 Dec;52(11):e13877. doi: 10.1111/and.13877. Epub 2020 Oct 30. PMID: 33125779.
- Sakkas D, Alvarez JG. Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil Steril. 2010 Mar 1;93(4):1027-36. doi: 10.1016/j.fertnstert.2009.10.046. Epub 2010 Jan 18. PMID: 20080235.
- Agarwal A, Majzoub A, Baskaran S, Panner Selvam MK, Cho CL, Henkel R, Finelli R, Leisegang K, Sengupta P, Barbarosie C, Parekh N, Alves MG, Ko E, Arafa M, Tadros N, Ramasamy R, Kavoussi P, Ambar R, Kuchakulla M, Robert KA, Iovine C, Durairajanayagam D, Jindal S, Shah R. Sperm DNA Fragmentation: A New Guideline for Clinicians. World J Mens Health. 2020 Oct;38(4):412-471. doi: 10.5534/wjmh.200128. Epub 2020 Aug 6. PMID: 32777871; PMCID: PMC7502318.
- Bungum M, Bungum L, Giwercman A. Sperm chromatin structure assay (SCSA): a tool in diagnosis and treatment of infertility. Asian J Androl. 2011 Jan;13(1):69-75. doi: 10.1038/aja.2010.73. Epub 2010 Nov 8. PMID: 21057512; PMCID: PMC3739398.
- Evenson D, Wixon R. Meta-analysis of sperm DNA fragmentation using the sperm chromatin structure assay. Reprod Biomed Online. 2006 Apr;12(4):466-72. doi: 10.1016/s1472-6483(10)62000-7. PMID: 16740220.
- Isoyama R, Kawai S, Shimizu Y, Harada H, Takihara H, Baba Y, Sakatoku J. [Clinical experience with methylcobalamin (CH3-B12) for male infertility]. Hinyokika Kiyo. 1984 Apr;30(4):581-6. Japanese. PMID: 6485962.


